Client Requirements
The client has an AI-powered clinical assistant product that automates essential cognitive workflow tasks, including triaging, patient engagement, and booking. However, they needed help scaling their operations and meeting the needs of their growing customer base. It is a product that provides a seamless healthcare experience for patients and providers. The client has limited clinics that operate with them now, but after the proposed requirement is done, they look forward to onboarding more clinics on their system.
Clients wanted us to develop a solution allowing them to scale their operations. Clients wanted to meet the needs of their growing customer base. Clients wanted to automate the current manual referral process. They also wanted to automate Medical Claim Management.
They also wanted Invoice generation and online and offline payment features. Also, they wanted to sync patient details with multiple EMRs. The client wanted to migrate to microservice-based architecture from the current PHP Application he used.
Thinkitive Solution
Thinkitive created a team of Product Managers, Senior QA analysts and System architects. Thinkitive understood the fundamental requirements of the client, created a list of non-functional requirements and the estimated time for each requirement along with the end-to-end functional flow and got it cleared from the client.
Thinkitive created the software specification document, high-level wireframes and user stories, and the client verified the test scenarios. Hence, the client understands the complete product before the product development starts and gets the change requests curated before starting the development.
Thinkitive started creating an architecture for the entire application suite for the product. Thinkitive created EPICs and User stories as a baseline to plan for a solution. Thinkitive delivered all the planned releases with little to no delays. Then we moved to production, and Thinkitive maintained the maintenance of the production application along with a team with minor enhancements, bug fixes and new feature development.
Solution Highlights
-
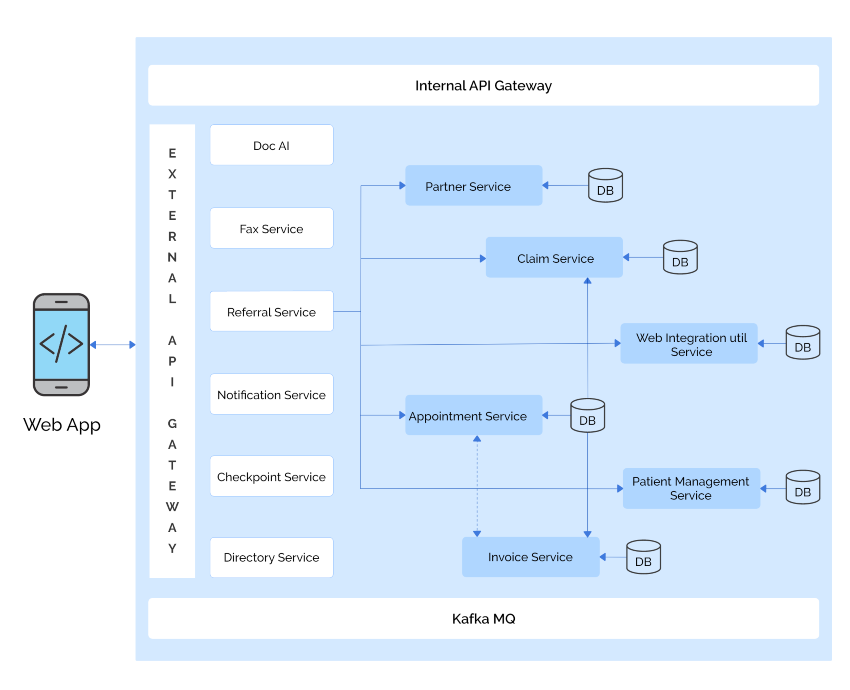
A Set of new microservices were developed under the guidance of the Software Architect, which can be plugged in with the existing system to serve the purpose and with the backward compatible architecture to ensure the current application flow stays untouched.
-
A machine learning AI model was developed using Python and trained on a large data set of Referral documents collected from the client to extract the data and tag them with the appropriate field. Each page was tagged with the appropriate label: Cover letter, Insurance Info, Patient Info and so on.
-
A referral microservice was developed to process all the incoming referrals and save them in various worklists according to their status. The referral service created the appointments for the selected location by the patient.
-
Claim service was introduced to process the insurance provided by the patient in the referral creation API; for processing the Claim, we used a 3rd party API which will take the procedure details that are mapped on both of the systems and will pass the procedure details to the required insurance provider and get the status of the status promptly. The response from the 3rd party API was being triggered in real-time, and based on that, and the updates were provided in the patient chart and in the notification of the Application in real-time.
-
The invoice was created as soon as the appointment for any procedure was created. Initially, the cost of each procedure was taken from the clinic and updated if the patient used insurance. The amount was calculated based on the patient responsibility received from the claim API response.
-
The existing Application, which was following a monolithic architecture, was converted to microservice architecture and different microservices were formed according to their functional requirements.
Value Delivered
-
The referral fax data extraction using the AI model auto-fills the referral form, and the clinic staff can only focus on verifying the inputted data and easily create the referral in no time.
-
The insurance was processed automatically, and the final reports came with real-time updates. The notification of the insurance eligibility was passed directly to the patient with a form link to add another insurance detail in case the submitted insurance expired, and the same process was followed again to know the eligibility and patient responsibility. The clinic staff can now skip calling the insurance companies to know the Prior auth and patient responsibility details for the patient.
-
As soon as the appointment was finished, the payment link was sent over the sms and via a notification to both the desk attendant and the patient for the final bill settlement. If any patient wants to make a card payment, the desk attendant would update the payment status or process the payment using the patient’s credit/ debit card.
-
The clinic could see the real-time patient detail updates, appointment creation, task creation and document upload in the EMR they were using. The clinic was easily creating the referral with the automated tools which we provided, and the same was updated on time in the EMR.
-
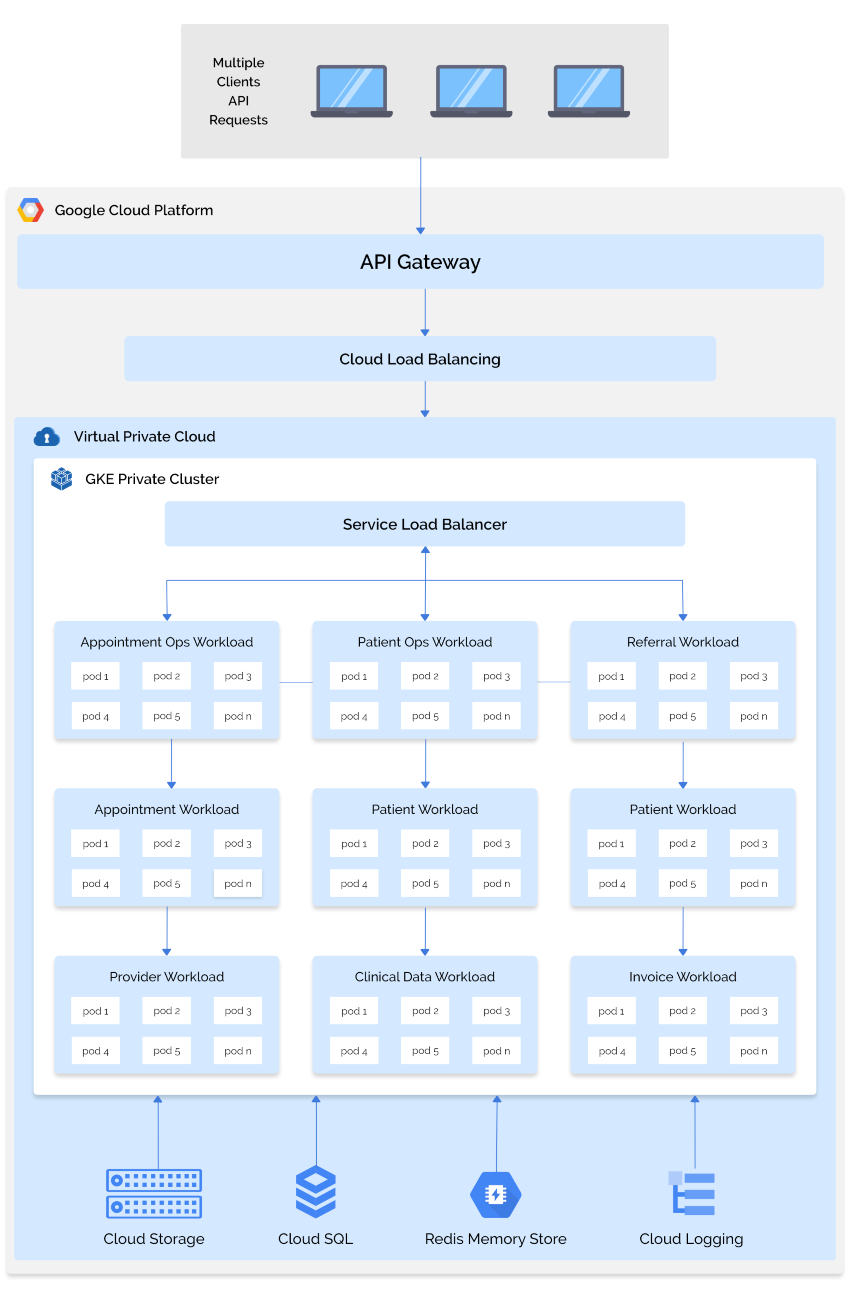
Using the microservice-based architecture, the upscaling of the microservices was quickly done if the load arose or any new clinic was onboarded. Then the required microservices instances were increased automatically using the flexible cloud architecture setup provided.
-
The clinic staff was now more focused on treating the patient well instead of crushed down into the pile of paperwork they had before.
Technologies and tools
-
Infrastructure: Cloud-based infrastructure using GCP
-
Kubernetes Engine, Compute Engine API, Yaml, Cloud Storage, Redis, Cloud Datastore API, IAM Service Account Credentials API, Cloud Run Admin API, Cloud Logging API, Ingres.
-
Backend: Nodejs, Express js, Python, TypeScript.
-
Database: Redis, MongoDB, MySQL.
Technical architecture Diagram Automating Workflows and Scaling Applications for Healthcare Service Provider Company