Overview
The client is a prominent US-based ophthalmology organization with a rich legacy spanning over two decades. Operating multiple clinics across diverse locations, they stand out as a leading specialist in ophthalmic care. With a substantial team of experienced ophthalmologists with a weekly patient capacity of 650 - 700 individuals. This organization is committed to providing cutting-edge eye care services. The organization has earned a stellar reputation for its commitment to innovation, patient-centric approach, and excellence in the field.
Business challenges
Ophthalmology Clinic, a multi-specialty ophthalmology practice, aims to streamline its billing processes and enhance accuracy in managing patient records. They seek an EMR solution tailored to ophthalmic care with comprehensive billing functionalities.
This organization's primary issues with the medical billing procedure include Complex Billing Requirements, Reimbursement Issues, and Compliance and Regulations. The client wants to streamline billing processes, improve revenue cycle management, and ensure compliance with complex healthcare billing regulations.
Thinkitive Solution
A group of SMEs and business analysts connected with the clients multiple times to obtain all the requirements. The team has created a feature list that outlines the project scope based on the information acquired about the client's requirements. The client was shown that feature list, and after a few modifications, we received their approval.
Our team has developed several essential elements that assist medical practitioners in streamlining their medical billing procedures. Additionally, the client was looking for explicit house integration, which helps to make claim submission easier.
- Ophthalmology-specific CPT Codes
- Seamless Clearinghouse integration
- Simplified Insurance Verification and Claims Processing
- Revenue Cycle Management
Development Approach
-
a) Requirement Gathering
The initial step involved gathering requirements from clients. Based on these requirements, we developed low-fidelity wireframes. Additionally, we conducted extensive consultations with ophthalmologists, billing specialists, and administrative staff to comprehend their specific needs and workflows.
-
b) Agile Development
We implemented an iterative development approach for this project, allowing for ongoing feedback and adjustments throughout the development process. It helped us to developed a very robust billing system.
-
c) Testing and Quality Assurance
Our development approach is milestone-based. Once we completed our milestone, we initiated the testing phase for the code. Rigorous testing was conducted for functionality, security, and user experience to ensure the creation of a robust and reliable system.
-
d) Training and Ongoing Support
After implementation, we offer continuous support to our clients. We provide comprehensive training to staff for seamless adoption and offer ongoing technical support following the implementation phase.
Solution Highlights
1. Ophthalmology-specific CPT Codes
The provider faced challenges while selecting appropriate CPT codes for the provided treatment. We have developed a secure database within EMR to store ophthalmology-specific CPT codes with descriptions. This database contains an extensive list of CPT codes for various ophthalmic examinations, treatments, and surgical procedures.
- Database Integration
- Auto-populated CPT codes with a description
2. Clearinghouse Integration
Integration with the clearing house will be beneficial in getting a higher reimbursement rate. Our team has delivered a feature that streamlines the clearing house integration process. Integration of the EMR system with a clearinghouse is possible using secure APIs.
We have developed a mechanism that helps to translate and map data from the EMR system to the required format for clearing house claim submission. Getting feedback from the clearing house regarding claim acceptance, rejection, and required modifications is possible.
- API Integration
- Data Mapping and Translation
- Error Handling and Feedback
- Batch submissions
3. Simplified Insurance Verification and Claims Processing
To increase reimbursement rates, it is essential to verify insurance before proceeding. In our developed and delivered feature, we have provided this real-time verification functionality with the insurance database integration.
The developed feature makes generating and submitting claims directly from patient records possible. Ensure claim information and the selected CPT codes are accurately included for submission. Also, we have provided a feature with a claim tracking system that helps you get all claim-related updates.
- Real-time Verification
- coverage details
- co-payments prior to appointments
- Automated Claim Submission
- Status Tracking
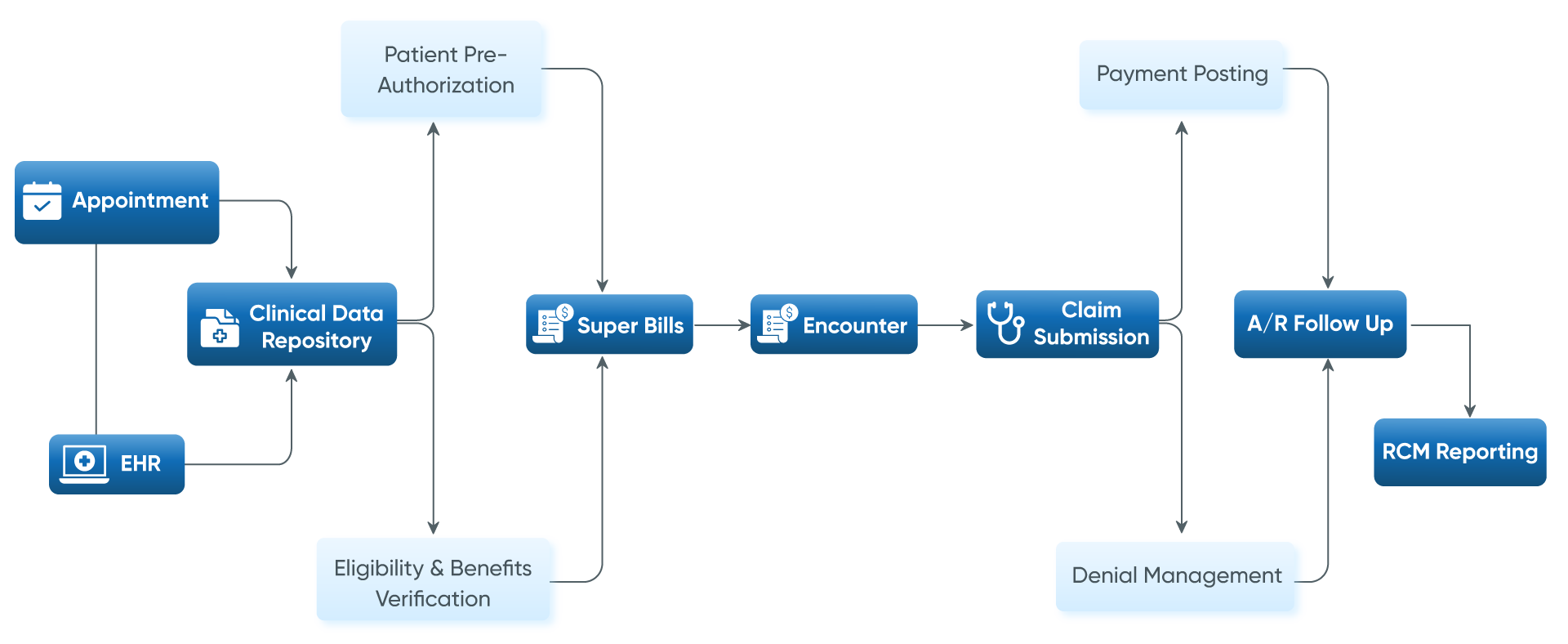
4. Revenue Cycle Management
The practitioners generally face challenges while maintaining records for claims and charges for provided services. To smoothen this process, we have offered a feature with the implementation of comprehensive charge capture functionality within the EMR. It helps record provided services, including CPT codes, service dates, and billed amounts.
Also, we have provided tools that allow easy integration with payment processing systems. Automatically post received payments to patient accounts and reconcile against submitted claims.
- Charge Capture Mechanism
- Seamless integration with payment processing systems
- Claim status
Value Delivered
-
Streamlined Billing Procedures
The provided features will assist in streamlining billing procedures with enhanced accuracy and efficiency in billing, reducing errors and delays in claim processing. The clinic experiences enhanced efficiency in managing patient billing while adhering to regulatory requirements.
-
Enhanced Operational Efficiency
Implementing delivered medical billing features will reduce administrative burden and improve workflow efficiency for the client's staff.
-
Improved Revenue Cycle
Specialised billing features will improve the revenue cycle by efficient charge capture, resulting in improved cash flow and reduced claim denials.
-
Compliance Adherence
Using the provided feature will not only assist in making the billing process more efficient but also maintain compliance adherence.
