Overview
We were approached by a client seeking to streamline their billing processes by incorporating a billing feature directly into their Electronic Health Record (EHR) system. Currently, the client relies on third-party tools for billing, which charges a percentage fee on received payments or margins. Despite servicing numerous patients and conducting multiple encounters, the client finds themselves giving away a significant portion of their profits.
To overcome these challenges, the client wanted a custom EHR software with an incorporated billing module. Furthermore, the client wanted the EHR system to include all billing-related functionalities like insurance verification, claims submission, which will allow them to manage all the billing-related tasks in-house.
Business challenges
1. Reliance on Third-Party Systems:
Managing billing through disjointed third-party tools and systems leads to inefficiencies and data fragmentation.
2. High Transaction Costs:
The third-party billing tool charged a percentage fee on received payments or margins, resulting in substantial transaction costs for the client with each transaction.
3. Poor insurance verification:
Inaccurate or incomplete insurance information results in denied claims.
4. Inefficient medical coding:
Incorrect or non-compliant coding practices lead to rejections.
5. Reliance on Third-Party Systems:
Managing billing through disjointed third-party tools and systems leads to inefficiencies and data fragmentation.
6. Untimely claim submissions:
Delays in claims submission exceed payer deadlines, resulting in denials.
Solution
Based on the collected client requirements, the team crafted a feature list defining the project's scope. Following refinements, the feature list was presented to the client and received approval.
In accordance with the approved feature list, our team began the development of a comprehensive EHR solution for the client. Below are the solutions we proposed to address their needs:
1. Comprehensive Billing Module within the EHR:
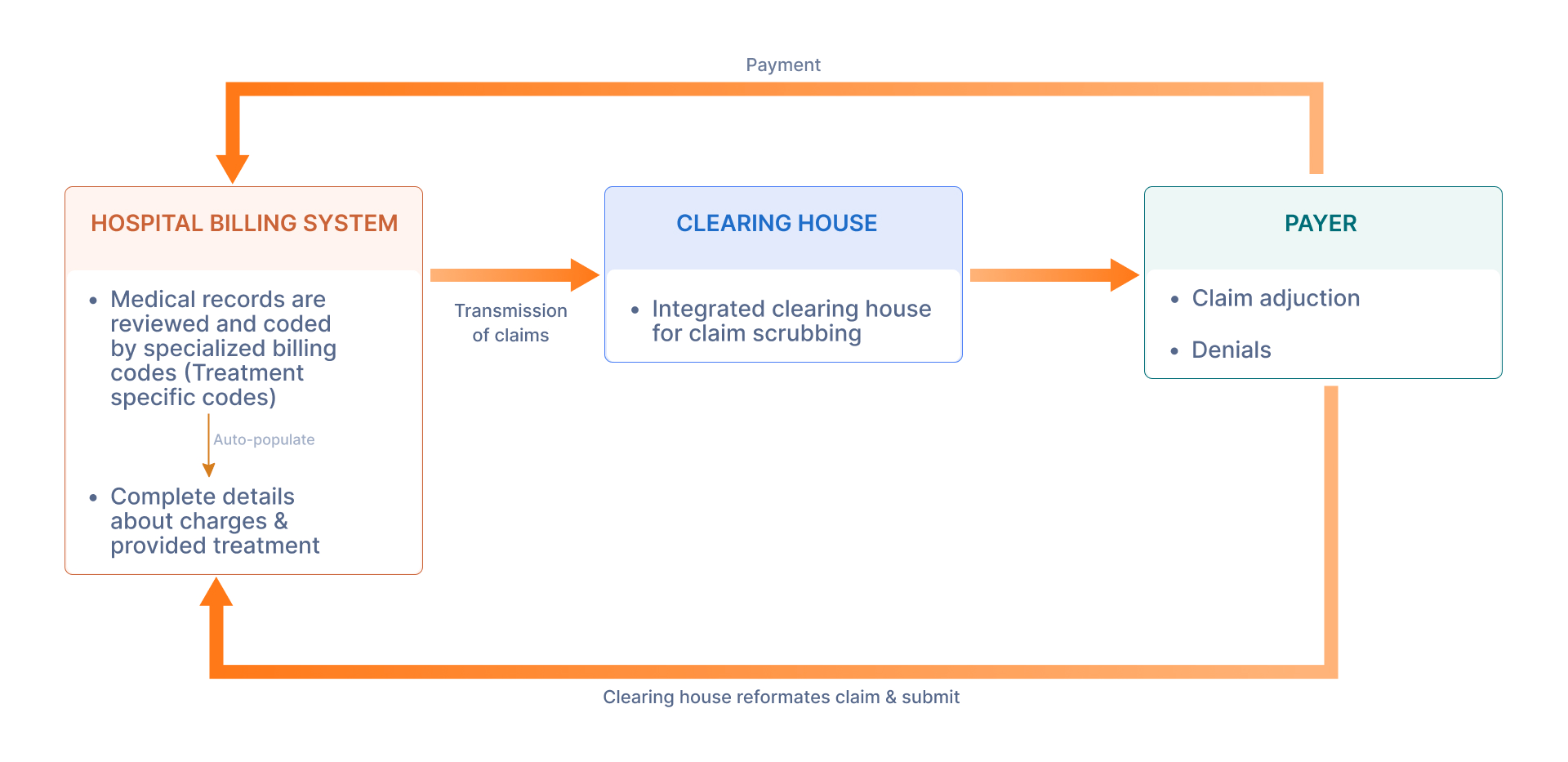
Our team has developed a comprehensive billing module within the EHR system to centralize billing operations and eliminate reliance on disparate third-party tools. Ensuring seamless integration with external billing systems or clearinghouses to facilitate data exchange and streamline billing workflows. Also, we have provided customizable billing templates and workflows to accommodate the unique needs of different clinics and specialties.
2. Integrated Insurance Verification:
The client experienced a high claim denial rate due to an ineffective insurance verification process. We have offered the integrated insurance verification and eligibility feature that helps you get a complete real-time verification report with coverage details. Getting coverage details with more accuracy helps reduce claim denials.
- Real-time eligibility check
- Coverage analysis
- Easily generate eligibility reports
- Facilitated Prior Authorization Support
3. Automated Coding and Compliance Tools:
We have Integrated advanced coding features into the EHR system, including built-in code lookup tools and coding assistance functionalities. We have provided customizable code libraries tailored to various medical specialties to streamline the coding process. Also, the team has implemented coding validation checks to identify and correct errors in real-time, minimizing the risk of coding-related claim denials.
- Auto-populate CPT codes
- CPT codes with description
- Map CPT codes with ICD-10 codes
- Customizable set for coding (Treatment specific codes)
4. Automated Claim Submission
Most of the time, claims get denied due to incorrect details for claim submission. To tackle this situation, we have offered a feature that automates claim submission. Integration with respective insurance facilities makes it possible to submit a claim without human errors. It ensures that claims are accurately and promptly sent to insurance providers.
5. Claim Denial Management (AI module)
To get minimum claim denials, we have delivered a feature incorporating artificial Intelligence (AI) and Machine Learning algorithms to analyze patterns in denials, predict potential issues, and suggest corrective actions. Integration with EHR ensures that we have collected correct patient and billing information and minimized errors in claim submission, resulting in fewer claim denials.
- Identification in denials
- Analysis and appeals
- AI incorporation
Value Delivered
-
Decrease in overall claim denials:
Integrating real-time verification, automated coding compliance checks, and claim scrubbing significantly reduces errors and omissions that lead to denials.
-
25% improvement in first-pass claim acceptance rate:
Streamlined electronic submission and automated error detection ensure claims are submitted accurately and accepted by payers the first time around.
-
20% reduction in time spent on billing tasks:
Streamlined workflows and automation free up staff time from tedious manual tasks, allowing them to focus on patient care and other critical activities.
-
Improved data accuracy and consistency:
Integrated systems and standardized processes minimize data errors and ensure consistent information across all aspects of the billing cycle.
-
30% increase in revenue collection:
Reduced denials and faster claim acceptance translate to faster and more complete reimbursement from payers.
