Simplify Process to Improve Finances with Revenue Cycle Management Software
Develop revenue cycle management software specific to your practice and simplify complex financial processes to improve your practice’s financial health.
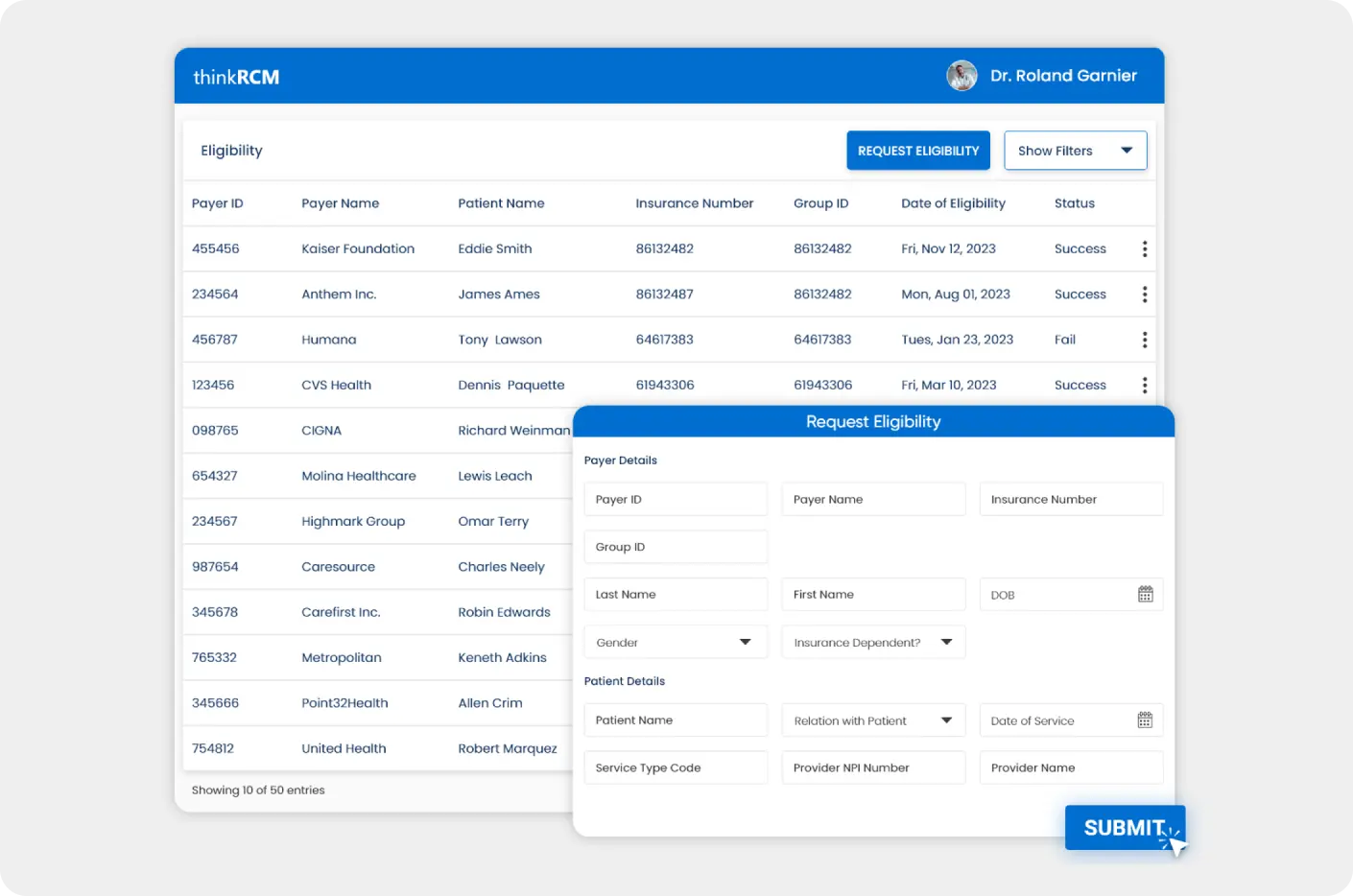
Verify patient insurance coverage from the software to minimize the risk of claims denials and streamline reimbursement with pre-authorizations.
Simplify medical coding with automated CPT code suggestions, real-time code validation and improve finances with superbilling processes.
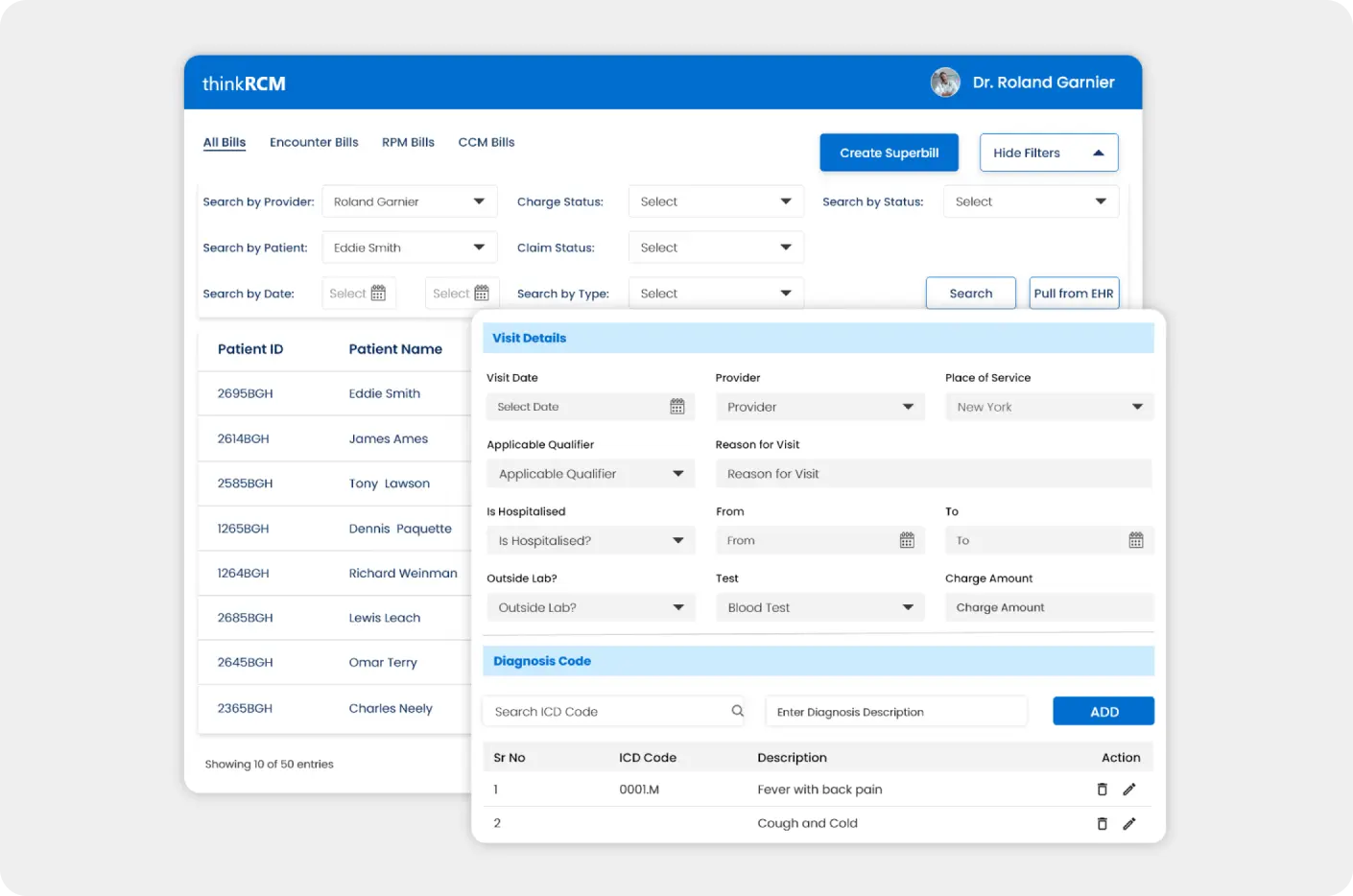
- AI Assisted Medical Coding
- Automated Data Capturing
- Automated Superbill Generation
- EHR Integration to Fetch Encounter Information
- Exportable Format Invoice Generation
Accurate and efficient billing processes with hands-free claim submission along with real-time denial management features.
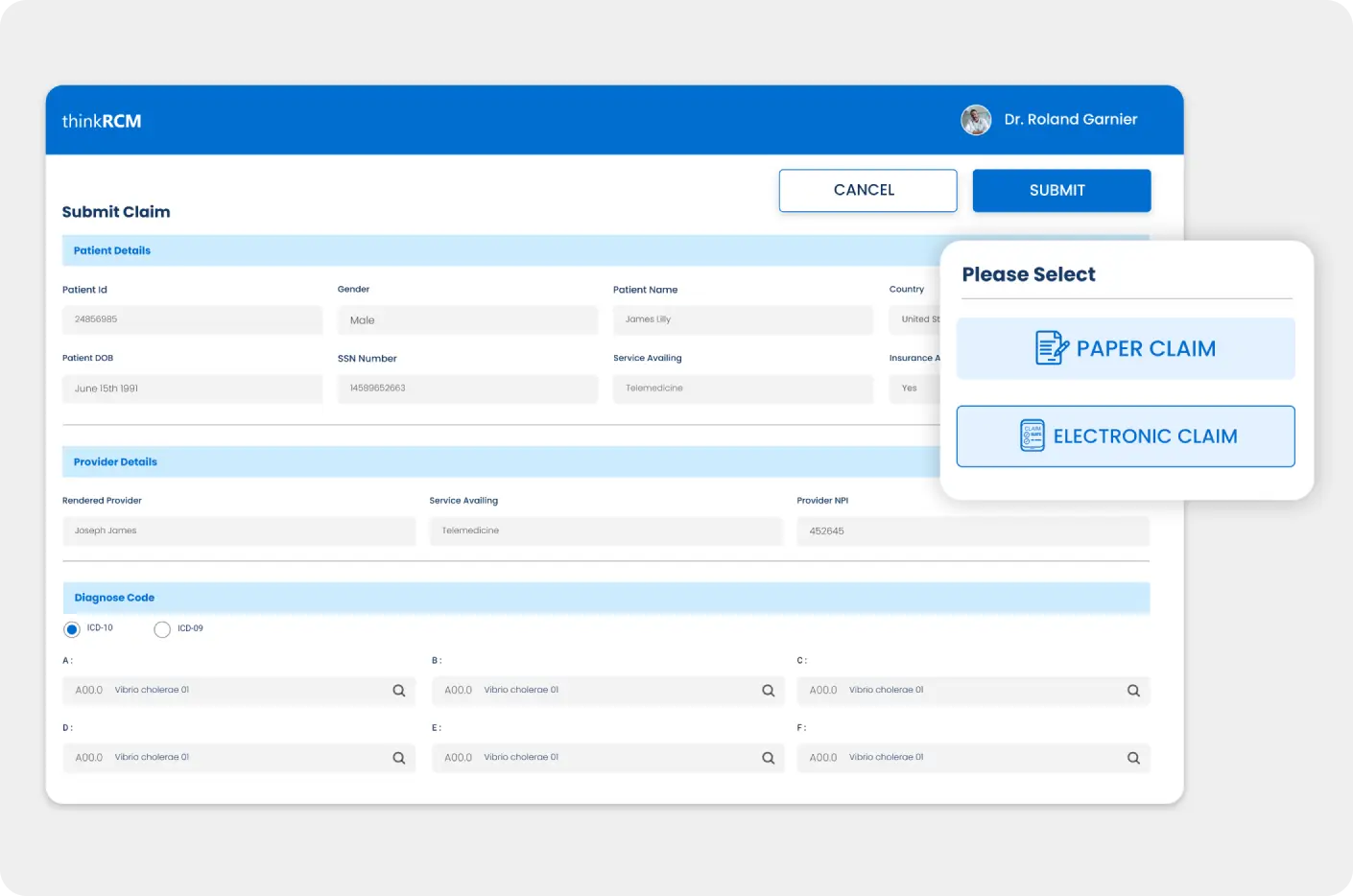
- Automated Information Filling and Single-Click Claim Submission
- Automated Claim Scrubbing
- Electronic Paperless Claim Submission
- Easy Claims and Reimbursement Tracking
- Actionable Denial Analysis and Claim Resubmission
Real-time ERA/EOB tracking and reporting to identify and manage claim and payment discrepancies.
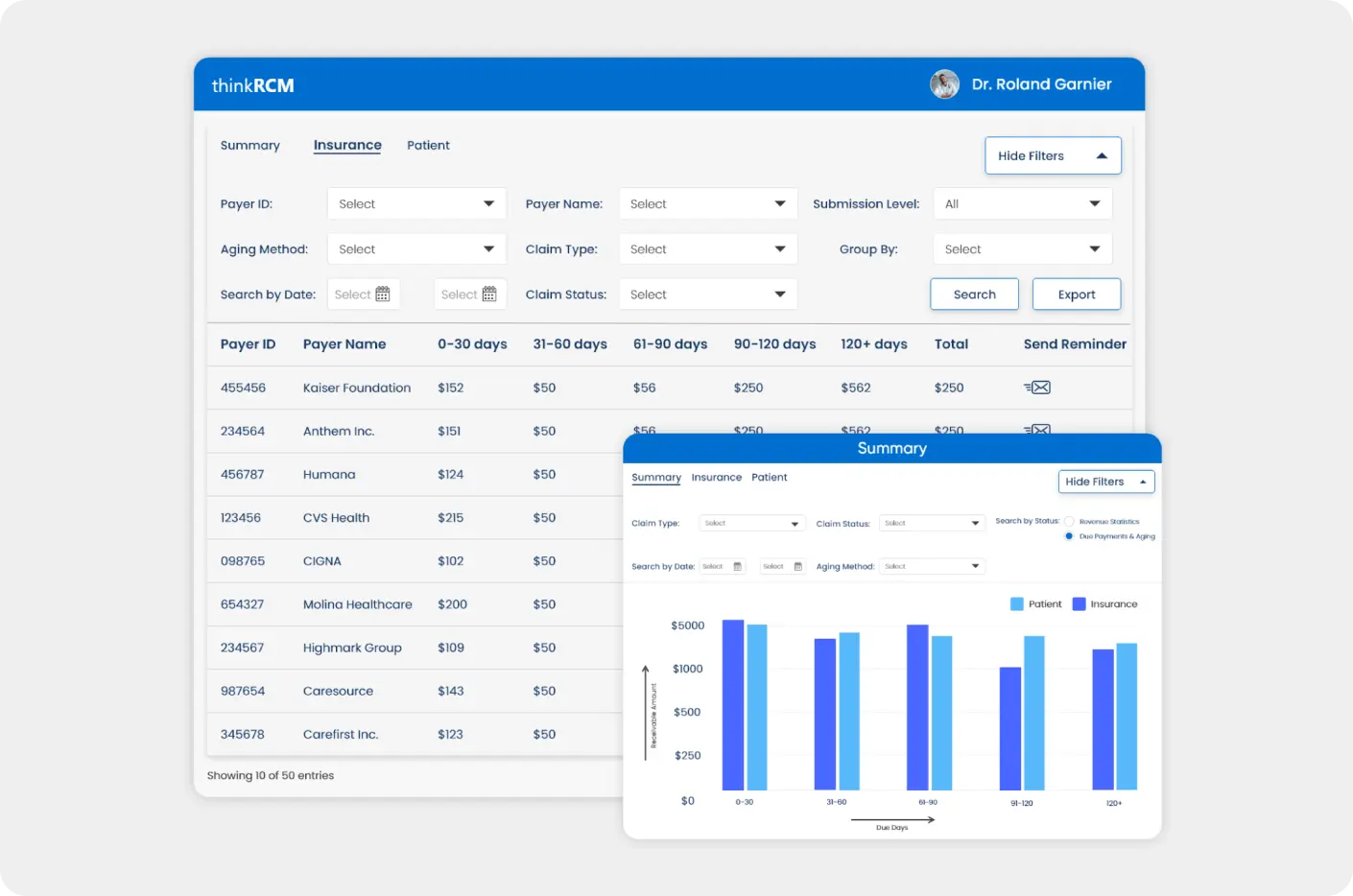
- Payment Status and Due Tracking
- Automated Reminders for Due Payments
- Custom Payment Policy
- ERA Payment Posting
- Automated EOB Posting
Generated automated reports on your practice’s finances to identify and address gaps to improve your practice’s financial performance.
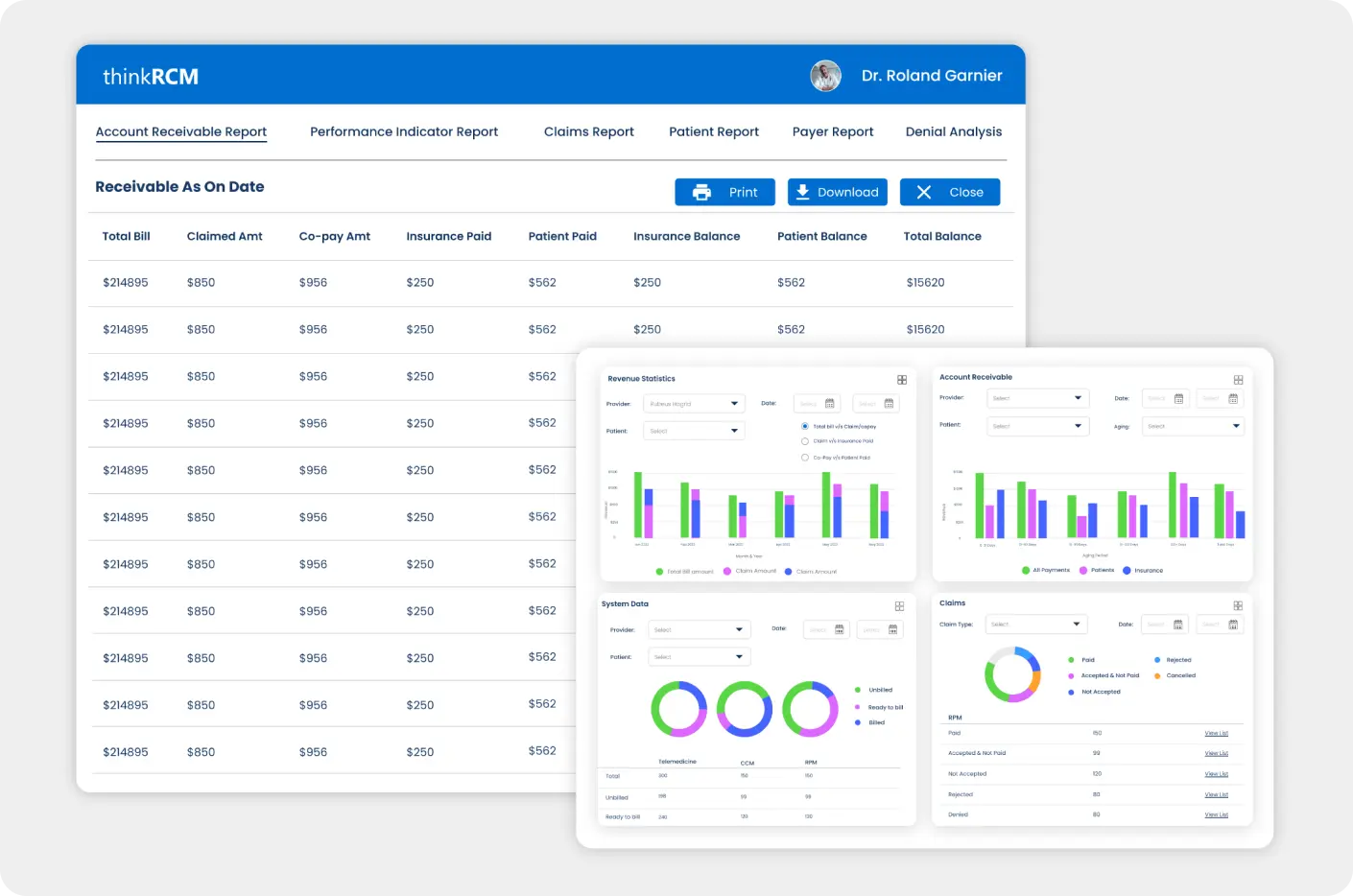
- Comprehensive and Informative Dashboards
- Performance Indicators to Identify Revenue Gaps
- Multiple Format Reporting with Graphs, Listicles, etc
- Automated Report Generation and Presentation
- Export Reports in XLS, PDF and CSV Formats
Streamline financial workflows with accuracy, transparency and visibility to improve revenue cycle processes and financial health.

- Real-time Information Pulling with EHR Integration
- Clearinghouse Integration to Reduce Denial Rate
- Payer Integration for Insurance Verification and Authorization
- Multiple Payment gateways
- HIPAA-Compliant Electronic Claim Transfer

Trust 125+ Clinics and 1465+ Providers Who Entrusted Thinkitive!
Thinkitive automates processes to save time and money.







Clients Testimonials
Join 150+ Happy Clients: See What They Have to Say
We've successfully collaborated with 150+ satisfied clients, and 95% of them have expressed their satisfaction with our medical software development company.
Cost & Timelines
Timely & Affordable Healthcare RCM Software Development
We deliver secure and feature-rich custom healthcare software solutions within your budget and set timeframe.
Complexity
Software complexity (its functionality scope)
Type
Software type (e.g. web, mobile, desktop)
No. of Users
The expected number of users
Integrations
The required integrations as per regulations
Compliance
Regulatory compliance requirements
Security
Performance, security, usability and accessibility requirements
Deployment
The chosen deployment model (e.g. on-premise, cloud)
Sourcing
The sourcing model (in-house, outsourcing) & team composition
We deliver healthcare software in the following timeframes
1 Week
Medical software project starts within 1 week
2-4 Months
MVP release
Every 2-4 Weeks
New healthcare software versions

Need a Tailored Healthcare RCM Software Cost Estimation?
Just answer these simple questions prepared by our consultants - it won’t take long.
Case studies
Transforming Success Stories of Healthcare RCM Software Development
Empowering Healthcare Technology Innovation
250+
Healthcare Projects
400+
Healthcare Experts
98%
Client Retention Rate
150+
Healthcare Customers
50%
Cost Saving on Development
Engagement models
Affordable & Flexible: Engagement Models for Every Need
Our flexible engagement models allow us to customize our services to meet your unique needs. Whether you're looking for a dedicated team, project-based work, or ongoing support, we have the right solution for you.
I have a requirement and want
to pay a fixed price
Share your project requirements, and our team will conduct a discovery call to understand your needs in detail. We'll provide a clear project estimate and deliver high-quality work. Pay only upon project completion and your satisfaction, ensuring you're never overcharged.
I want to hire a healthcare software developers
on an hourly basis
Hire dedicated developers with 160 hours of focused attention each month. Enjoy peace of mind with transparent billing, daily timesheets, and our unwavering commitment to your success. Benefit from the expert guidance of our complimentary Delivery Manager.
SAVE
EXTRA 20%
Specialties
Specialty-Focused Healthcare RCM Software Development
Customized healthcare RCM software tailored to the unique needs of healthcare specialties.
Unlock Practice Potential with Specialty-Specific RCM Software
Check how our custom RCM software assists and supports your specialty in action.
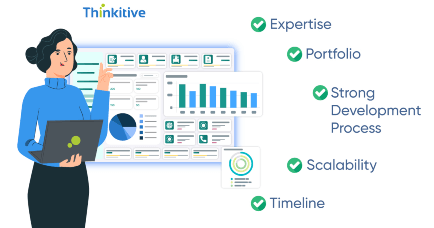
To Develop Custom RCM Software Development
Domain-specific Accelerators & Frameworks
End to End Healthcare Digital Transformation
Interoperable Data systems
Assured Compliance & Security
Proficiency in Healthcare Standards
AI & Analytics Powered App Insights
Pre-Built Components
Build Your Custom RCM Software Rapidly by Leveraging Pre-Built Components
Every specialty has unique needs in medical billing, practice management, and EHR solutions.
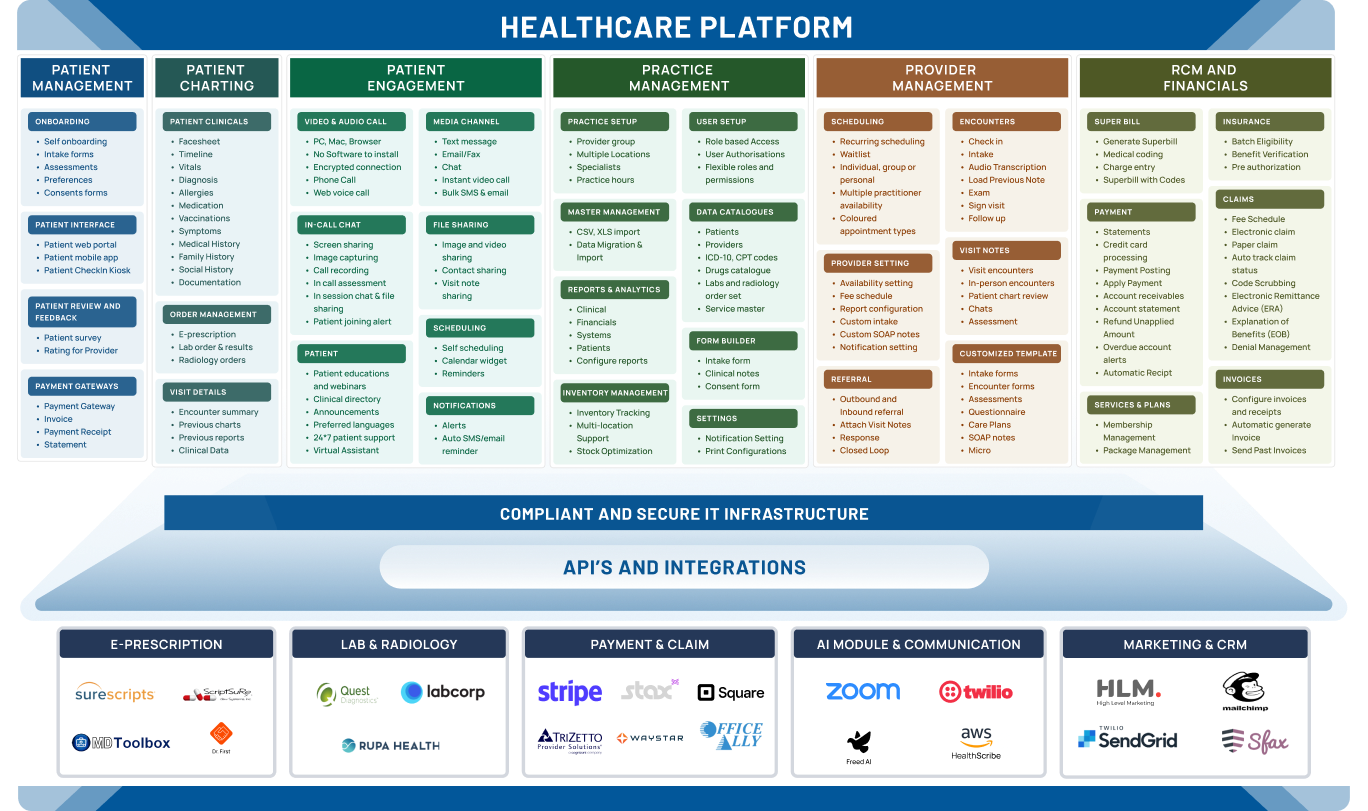
Integration
API-based Connectivity through our Robust Integration
ePrescription & Labs Integration
We provide custom healthcare software development ... services with ePrescriptions and Labs integration to enable you to send orders directly from the healthcare system. These integrations offer multiple benefits, from reducing errors to improving clinical efficiency and reducing the overall cost of care for both patients and providers.

Surescripts
Surescripts is the leading ePrescription network that helps improve medication ... safety and convenience for patients, providers, pharmacies, and payers. Integrate Surescripts during custom healthcare RCM software development to enable secure electronic ePrescription and real-time access to patient medication history.
Billing & Payment
Safe, secure, and seamless healthcare transactions with our billing, ... payment, and point-of-sale integrations into your custom healthcare software solutions. Give your virtual care practice a comprehensive real-life healthcare ecosystem.

Waystar
Waystar provides healthcare revenue cycle management solutions. Streamline claims processing, reduce denials, and optimize revenue capture through automation and AI, improving financial efficiency for healthcare organizations with Waystar.
Communication
Facilitate real-time communication with patients via various ... media, all from your custom healthcare RCM software solution. Give your virtual care practice a comprehensive real-life healthcare ecosystem.

Sfax
Sfax is a secure faxing solution designed for healthcare. Integrating it during healthcare web RCM app development enables secure exchange of patient information like faxes within the system, ensuring patient data privacy and compliance with HIPAA regulations. This streamlines communication and protects sensitive medical information.

Still chasing claims manually?
Let our RCM software handle it with faster billing, fewer errors, and better cash flow.







Framework & Technology Expertise
Our RCM Software Developers' Framework & Technology Expertise
Leverage the expertise of experienced healthcare software developers and healthcare software development teams in a wide range of technologies and frameworks.
Back-end Programming Languages
Front-end Programming Languages
Languages
Javascript Frameworks
Mobile
Cloud
Databases/Data Storages
SQL
NOSQL
Platforms
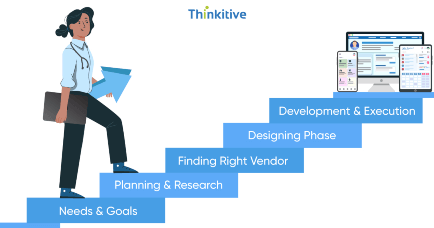
THINKITIVE’S HEALTHCARE SOFTWARE DEVELOPMENT PROCESS
Affordable Development Anytime, Anywhere
Our skilled healthcare software developers have expertise in understanding the unique clinical needs and requirements of the healthcare practice.
- Domain Expert
To understand clinical and end-user needs.
- Business Requirements
To make market-fit solutions.
- Wireframes & User flows
To define software functions and functionalities.
- Dynamic UI/UX
Elevated experience for patients and providers.
- Sprint Creations
To plan the healthcare RCM software development.
- Coding & API Integration
Software coding as per necessary compliances.
- Manual Testing
For manually checking software functionalities.
- Automation Testing
Scripting for testing software functionalities.
- Rigorous Testing
End-to-end thorough testing of the software.
- Secure & Compliant
Ensuring the healthcare RCM system infrastructure is secure and HIPAA compliant.
- Integration
Application Integration for deployment.
- Maintenance & Support
User feedback and audits for continuous improvement.

Need to Design, Develop, or Improve
Healthcare RCM Software?







Frequently Asked Questions
Get answers to all your questions
Still have questions ?
To make sure data flows smoothly, it is important to integrate RCM software with the ERP systems. Some of the key considerations in this include:
- Data accuracy: Keeping information consistent across systems is known as data accuracy.
- Workflow optimization: Reducing human error by automating procedures.
- Real-time visibility: Offering a cohesive perspective of operational and financial data.
- Flexibility: Adjusting to changing industry standards.
- Security: Keeping private private patient and financial data safe.
Everything About Healthcare Software Development
Healthcare Software Development Blogs

Custom Healthcare Software for Population Health Management
The Role of Healthcare Software Developers in Digital Transformation
Benefits of Custom Healthcare Software for Small Practices & Clinics