Overview
Our client, a well-known psychiatric healthcare clinic operating across the US, focused on supporting individuals with different beliefs and identities through teletherapy. They specialize in treating Anxiety, Depression, Mental health concerns, Resolving conflicts in relationships, and addressing racial trauma.
Business challenges
The organization mainly faces challenges in the medical billing process, including complex coding and billing requirements, insurance verification issues, management of claim denials and rejections, and real-time eligibility verification. Despite being busy, the clinic faces problems with getting bills right, working efficiently, and following rules properly. Handling psychiatric services manually leads to mistakes in billing, causing delays in payments and more work for the staff. The client contacts us to streamline their medical billing process and improve the efficiency and accuracy of the insurance claiming process.
Thinkitive Solution
A group of SMEs and business analysts collaborated with clients to obtain all the requirements. The team has created a feature list that outlines the project scope based on the information acquired about the client's requirements. The client was shown that feature list, and after a few modifications, we received their approval.
We utilize agile development methodologies to build the EMR system in iterative stages, focusing on core functionalities such as secure patient data storage, appointment scheduling, and billing integration.
The development team got to work on the project following the requirements. Our team has developed several essential elements that assist medical practitioners in streamlining their practice procedures. We have offered some of the key features-
- Billing integrations
- Specialized billing codes
- Seamless insurance verification and eligibility
- Automated claim submission
- Claim denial management
Solution Highlights
1. Billing Integration
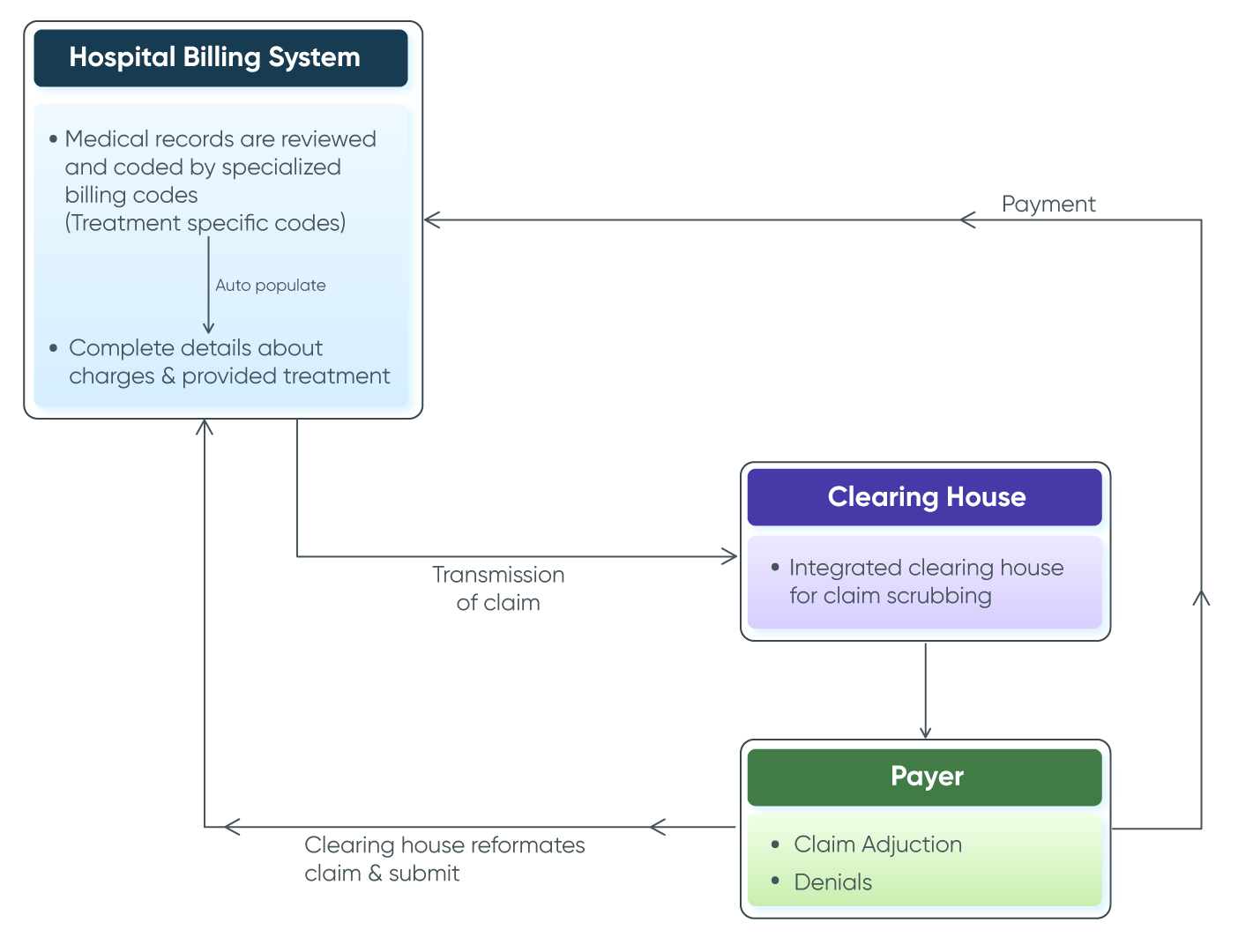
We have developed a billing module that seamlessly integrates with psychiatric documentation, ensuring accurate coding and facilitating efficient claims submission. We incorporated new codes into their current EMR software and integrated the system with a clearinghouse (Optum). This integration helped minimize errors and decreased the need for manual work when filing and submitting claims.
2. Specialized Billing Codes
The provider faced an issue applying accurate medical billing codes with complete undersSolution Highlightstanding. We have provided a specialized feature that helps provide a comprehensive range of psychiatric-specific billing codes. CPT codes auto-populate as per the diagnosis. This feature comes with more efficiency and accuracy in the billing process.
- Auto-populate CPT codes
- CPT codes with description
- Customizable set for coding (Treatment specific codes)
3. Seamless Insurance Verification and Eligibility
The client was getting claim denials due to an insufficient insurance verification process. We have offered the integrated insurance verification and eligibility feature that helps you get a complete real-time verification report with coverage details. Getting coverage details with more accuracy helps reduce claim denials.
- Real-time eligibility check
- Coverage analysis
- Easily generate eligibility reports
- Facilitated Prior Authorization Support
4. Automated Claim Submission
Most of the time, claims get denied due to incorrect details for claim submission. To tackle this situation, we have offered a feature that automates claim submission. Integration with respective insurance facilities makes it possible to submit a claim without human errors. It ensures that claims are accurately and promptly sent to insurance providers.
5. Claim Denial Management (AI module)
To get minimum claim denials, we have delivered a feature incorporating artificial Intelligence (AI) and Machine Learning algorithms to analyze patterns in denials, predict potential issues, and suggest corrective actions. Integration with EHR ensures that we have collected correct patient and billing information and minimized errors in claim submission, resulting in fewer claim denials.
- Identification in denials
- Analysis and appeals
- AI incorporation
Value Delivered
-
Enhanced Billing Accuracy
The system ensures that psychiatric treatments are accurately billed to minimize billing problems and possible revenue loss due to inaccurate billing.
-
Data-Driven Insights
Comprehensive reporting features offered insightful information for analysis, auditing, and decision-making to maximize overall financial performance and the billing process.
-
Efficiency in Claims Management
Automated claim submissions and denial management streamlined the billing process, reducing the administrative burden on staff.
-
Improved Revenue Cycle
The healthcare facility's revenue collection and financial stability increased due to reduced claim denials and effective revenue cycle management.
