Overview
The US-based client seeking assistance is a highly experienced healthcare professional with a decade of expertise in the urgent care field. Serving as the Chief Medical Officer at UrgentCare, they manage a network of multiple urgent care clinics situated in different parts of the United States. The client reached out to us with the goal of optimizing their revenue cycle management and enhancing the effectiveness of their billing and claims processing systems.
Business challenges
The client was using EMR software not integrated with the clearinghouse, leading to manual completion and postal submission of CMS1500 claim forms. As a result, digital tracking of claims status was unavailable, requiring increased administrative efforts.
The challenges faced by the client included inefficient claim processing, high denial rates, limited visibility, elevated costs, and revenue loss. To address these issues, the client sought integrated software with the clearinghouse.
Moreover, the provider expressed a need for seamless patient intake, AI-generated notes, telehealth capabilities, and patient alert management features. The client's goal was to enhance reimbursement rates and alleviate the administrative workload.
Thinkitive Solution
Thinkitive business analyst team and SMEs connected with clients to get complete requirements for software development. After connecting with the client multiple times, the team finalized the requirements. Based on the gathered client requirements, the team has developed a feature list that describes the project scope.
Based on the approved feature list from the client, the development team has started working on integration with the clearing house. As per requirement, the team has also started to work on additional features like patient intake, AI-generated notes, telehealth capabilities, and patient alert management.
Solution Highlights
-
Maintained data exchange standards (ANSI X12 or HL7)- To ensure system compatibility, we have maintained standardized data exchange formats.
-
Automatic Eligibility verification- The eligibility verification checks patient insurance eligibility before submitting a claim.
-
Pre Authorization- A process used to determine whether a specific medical procedure or service is necessary and will be covered by a patient's health insurance plan.
-
E-Claim submission - EDI (Electronic Data Interchange) is used in healthcare revenue cycle management (RCM) to exchange electronic documents between providers and payers.
-
Claim status update- The claim status file is used to check the status of a claim, including whether the claim has been received, processed, or paid.
-
Electronic Remittance Advice (ERA) - The payment/remittance provides payment details, such as the amount paid, any adjustments or denials, and the reason for the adjustment or denial.
-
Patient Statements - It generates patient statements and sends them electronically to patients.
1. Clearing House Integration
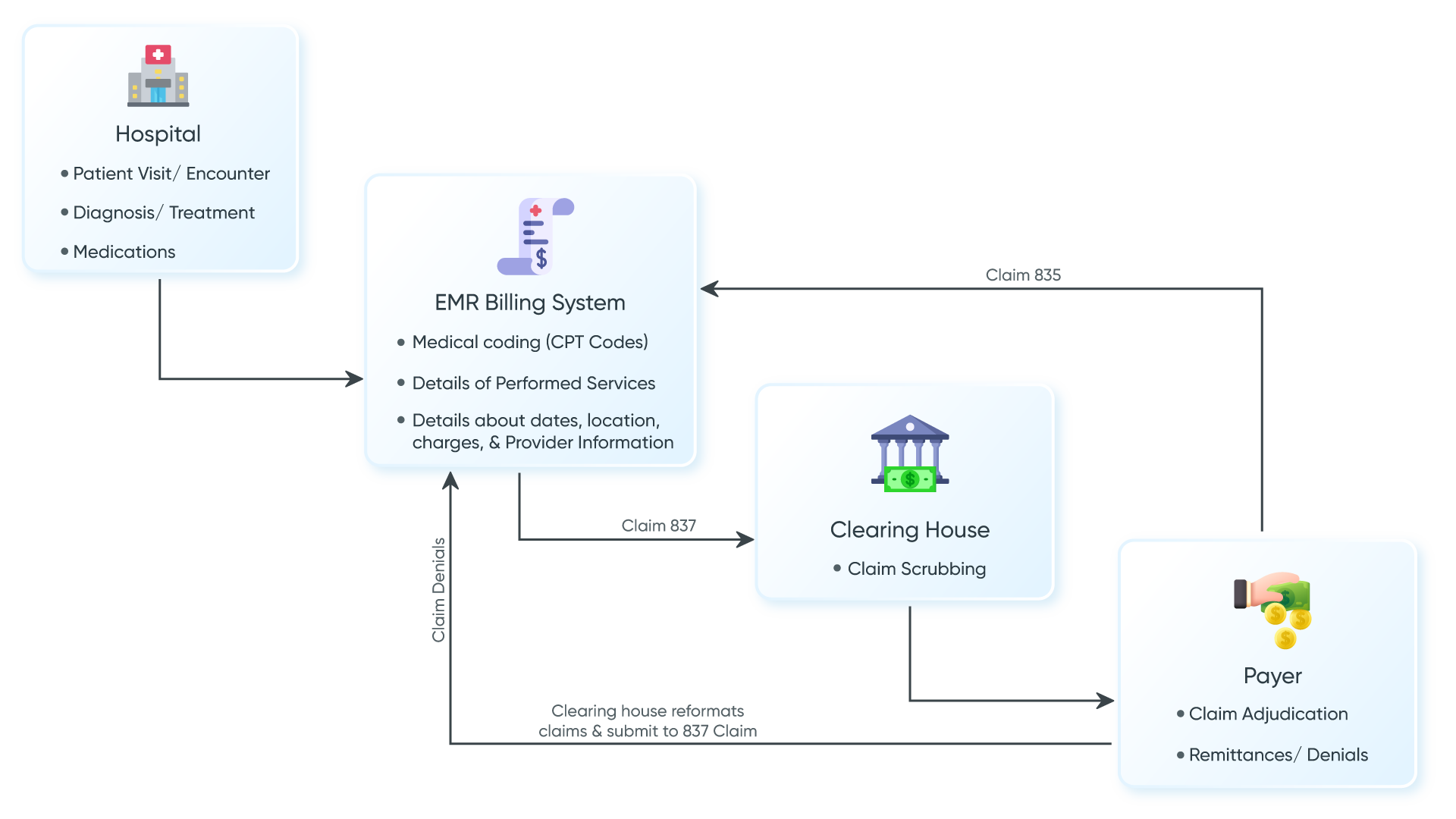
Clearinghouses are intermediaries between healthcare providers and insurance payers. Integration with a clearing house offers several features-
With the integration clearing house, clients solved the below problems
2. Patient Onboarding and Intake
It is possible to have a seamless patient onboarding and intake process with the help of the provided feature. Using a custom template, it is possible to collect essential patient data in a short time period.
3. AI-generated Automated Notes
During patient encounters, it is possible to complete SOAP notes with the help of AI features. When a discussion with a patient is happening, the system will capture audio and generate notes for the same.
- Audio capture for note generation
4. Telehealth Portal
Virtual consultation is helpful for those patients who are not able to visit the clinic but require care on an urgent basis. In this module, patients can have access to book their appointment slots at their convenience for a specific provider on virtual.
- Allows audio and video links for telehealth (Eligible patients)
5. E-Prescription
External integration with pharmacies using e-prescription assists in transferring prescriptions directly to pharmacies. Helps to reduce errors and make the process seamless.
Value Delivered
-
Raise In Reimbursement
Provided features help to reduce claim denials and assist in improving billing accuracy. The client noticed an increase in reimbursement rates, resulting in a significant boost to their revenue.
-
Instant Claim Processing
Billing with more efficiency and fewer errors will lead to processing claims more seamlessly. It helps reduce the time it takes to receive payments from insurance companies.
-
Reduced Administrative Burden
It is possible to complete multiple tasks with less time and more accuracy using features. Assists in reducing the administrative burden on staff members.
-
Financial Visibility
Integration with a clearing house helps get claims updates with a remittance feature. It is possible to get a clear idea about the approved claim amount.
-
Cost Saving
Integrating with a clearing house will be beneficial in terms of eliminating 3rd party dependencies. It helps to cut down costs and get more revenue.
