Legacy System Integration: Connecting Old and New Healthcare Software
Here is a number that might surprise you: 76% of healthcare organizations are still using multiple systems over a decade old for critical clinical operations. And these are not just the peripheral systems; they are handling billing, documentation, and almost everything from them.
We have all been there when your legacy healthcare systems freeze during an appointment scheduling or when you are in the middle of entering patient data. This then becomes a healthcare tech’s version of being stuck between a rock and a hard place.
Then, should you rip and replace everything from scratch? Not so fast, because the price tag for complete replacement would make any CFO break into a cold sweat. You need millions of dollars, months of implementation, operational disruptions, and multiple such time-consuming tasks.
But what if I tell you a better way to change this and get almost the same functionalities with a fraction of the replacement cost?
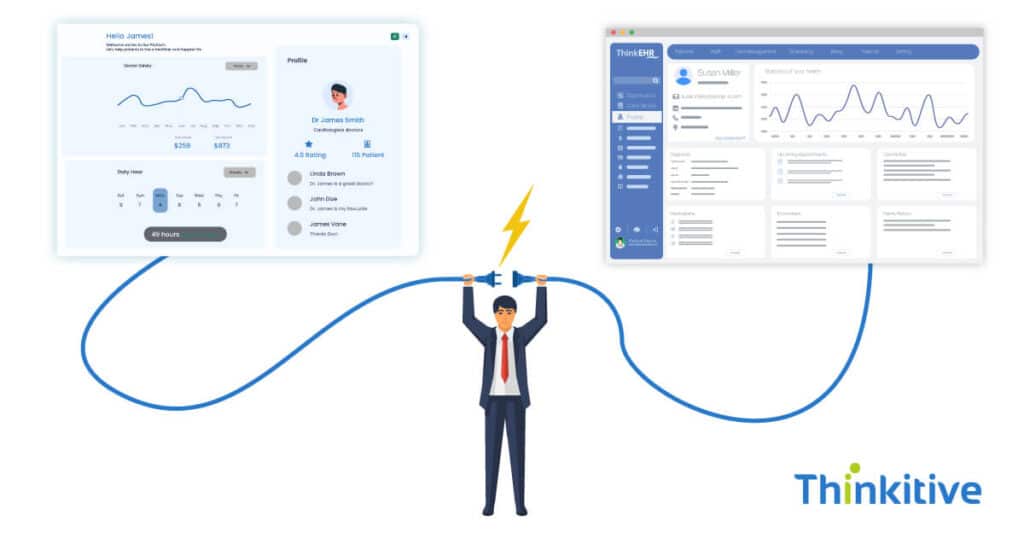
This way, you can modernize medical software and integrate your legacy systems with new EHRs. This article will show you the practical ways to transform your technology ecosystem without emptying your coffers or disrupting patient care.
Furthermore, you will know how organizations use API connections to make smoother EHR integration from new to old systems. Middleware solutions that bridge technological gaps and phased legacy data migration strategies that let you modernize your systems at your own pace.
Let’s discover how your organization can evolve without the trauma of a complete system transplant.
Current Healthcare Legacy Modernization
Modernizing legacy healthcare systems is no longer optional, it’s a strategic imperative accelerated by post-COVID digital transformation demands. Many legacy platforms lack interoperability, mobility, and security, creating friction in care delivery and compliance. Organizations are increasingly adopting cloud migration strategies and hybrid integration approaches that preserve core legacy functions while extending capabilities through APIs and microservices.
Legacy systems must also be brought up to speed with modern cybersecurity standards, including encryption, identity access management, and Zero Trust models to protect against today’s evolving threat landscape. Additionally, integration efforts must account for evolving regulatory mandates—including ONC’s Cures Act Final Rule, FHIR API requirements, and stricter HIPAA enforcement around data access, auditability, and consent. Successful modernization balances risk, cost, and long-term scalability while ensuring legacy systems remain functional, secure, and compliant.
Assessing Legacy System Integration Potential
Before diving into integration work, you need to know if your legacy systems are good candidates in the first place and what their healthcare system compatibility is. You can start by looking at what connectivity options you have available. Are there APIs in your older system, database access points, or at least file export capabilities? You will be surprised by how many legacy systems have hidden connection points that remain unexplored.
The next step is to check what documentation actually exists. There are systems that do not have complete documentation, making it difficult to solve the puzzle of connectivity, further adding to your discovery time.
You also need to know if the vendor who built the system is still available and what their charges are for changes in the system. Knowing this is important as it will decide whether they will be your allies or a hindrance to the system’s modernization.
Don’t skip security and data integrity considerations. Your legacy system might have been secure in 2005, but does it meet today’s standards when exposed through integration points? Performance impacts matter, too—will integration queries bog down systems that are already running at capacity?
When weighing integration versus replacement, identify the truly critical functionality you need versus the nice-to-have features. Calculate ROI by comparing integration costs against full replacement expenses, factoring in both immediate needs and technical debt. Remember that maintaining integrated legacy systems still carries costs—they won’t run forever without investment.
The right decision isn’t always obvious, but a structured assessment helps you avoid the costly mistake of trying to integrate systems that should be retired or replacing systems that could serve you well with proper integration approaches.
Technical Approaches for Legacy System Integration

Once you’ve determined integration is feasible, it’s time to pick your technical approach. Think of integration tools as translators between your old and new systems—they come in different flavors to match your situation.
If the budget allows, commercial healthcare integration platforms like Redox, Mirth Connect, or InterSystems HealthShare can save tremendous time. They come pre-built with healthcare-specific connectors and transformations. Short on funds? Open-source alternatives like HAPI FHIR or OpenHIM offer solid capabilities without the licensing costs, though you’ll invest more in configuration and support.
When direct connections aren’t available, get creative with your access methods. Sometimes, you’ll need to go straight to the database level (just be careful not to violate vendor agreements!). For truly stubborn systems, screen scraping might be your only option—not elegant, but it works when nothing else will. File-based integration using HL7, FHIR, or even good old CSV files can be surprisingly effective for systems that support batch exports and imports.
Need more real-time communication? Message queuing using RabbitMQ or Kafka creates reliable system-to-system pathways even when one system is temporarily unavailable.
Modern API approaches can breathe new life into old systems. Consider wrapping legacy functionality in REST APIs that newer applications can easily consume. If you’re dealing with older SOAP services, transformation layers can convert them to more accessible REST endpoints. For complex data needs, GraphQL implementations give consuming applications more flexibility in specifying exactly what data they need.
Remember, the best technical approach often combines several of these methods based on your specific systems and requirements—there’s rarely a one-size-fits-all solution in legacy integration.
Data Migration and Synchronization Strategies
Moving your data is the trickiest part of taking outdated EHR integration to a modern system. First, you’ll need to decide between a one-time migration and keeping systems in sync continuously. One-time transfers work when retiring a system entirely, while ongoing synchronization keeps parallel systems working together harmoniously.
What about your historical data? Do you need every single record from the past decade or just active patients from the last two years? Selective migration can significantly reduce complexity and cost. Remember that old database maxim: more data, more problems.
Planning your cut-over is crucial—will you switch systems over a weekend or gradually transition department by department? Each approach has different data synchronization requirements and risk levels.
If you’re maintaining bidirectional synchronization (data flowing both ways), prepare for some headaches. You’ll need clear rules for handling conflicts when both systems update the same record. Which system becomes the “source of truth” for each data element? How will you maintain transaction integrity when updates span multiple systems?
Don’t underestimate system-specific data quirks. That perfectly normal patient name in your legacy system might trigger validation errors in your new one. Run a thorough data quality assessment before migration, then develop transformation rules to handle anomalies.
Finally, validate everything after migration. Random sampling isn’t enough—create comprehensive validation scripts that verify record counts, key fields, relationships, and business rules. The peace of mind is worth the extra effort, and your clinicians will thank you when they don’t have to hunt for missing allergies or medication histories.
User Experience and Workflow Considerations

But getting the technical part right is only half the battle. If your clinicians have to handle multiple interfaces, remember different passwords, and do information transfer manually, they will be frustrated no matter how good your EHR system is at the backend.
So, to make this easier for your staff, start with a single sign-on implementation, as nothing kills productivity faster than entering passwords on different screens again and again. You can take this step further by using context-sharing between applications. So, when a nurse clicks on a patient in one system, the other applications automatically load that same information.
However, if you want a truly seamless experience, then using an embedded application framework directly lets you incorporate legacy functionality in your modern interfaces. But remember to know your workflows across your systems thoroughly before implementing any technical solutions.
This helps you find any redundant steps in the workflows and helps make them better. Additionally, when rolling out your integrated environment, doing it in a phased approach minimizes the disruptions in the transition.
Train super-users from each department who understand both the old and new workflows—they’ll be your front-line support and change champions. Develop cross-system training that focuses on complete workflows rather than individual applications.
Finally, don’t dismantle your support structure too quickly. Integrated environments create complex troubleshooting scenarios. This is why it becomes difficult to identify whether the issue is with the legacy system, the new system, or something else. Make sure your support team can answer this efficiently.
Security and Compliance in Legacy Integration
When you are blending legacy systems with modern healthcare technology, security and compliance can’t be just afterthoughts. Legacy systems were not designed with today’s cyber threats and regulatory compliance in mind, so integrating them means you are increasing the risk potential significantly.
Start with a full vulnerability assessment of your systems by probing your system for any security loopholes through penetration testing and static analysis. Then, your next step is to look at how these systems stack up in terms of authentication and authorization. As most legacy systems lack the ability and flexibility for modern identity management, and if your systems are isolated, then things can get messy quickly.
Along with all of this, you also need to track role mapping and access control synchronization if you want to avoid the troubles of unauthorized access. Here, the integration points, such as APIs, middlewares, and data exchange layers, are also important, and they all need a deep vulnerability scan.
After the scan comes the step to apply robust security measures like encryption, role-based access, or firewalls. These solid mitigation strategies keep your legacy systems safe during and after the integration. On the compliance side, adhering to HIPAA compliance is necessary, with every move audited and logged along with data integrity and complete documentation for regulatory validation.
Finally, you need to know that integration isn’t just about connecting systems; it’s about doing it securely, responsibly, and in a way that keeps you compliant without slowing you down.
Implementation Roadmap

Discussing integration is one thing, but actually seeing how it happens tells you the real practical story, and that is where the real learning happens. That is why looking at case studies makes it clear how different systems handle integration and implementation between legacy and modern systems.
For instance, a hospital that integrated its legacy system with a radiology lab and a pharmacy system into a new cloud-based EHR. But in this, they did not transfer all their data and system in a single go; they implemented a phased approach. By prioritizing critical workflows, such as, medication management and patient charting, first. This minimized their early-stage disruptions and kept the high-value systems running.
Conversely, a multi-speciality network used a pilot program approach. First, they chose one place to test the interoperability, fixed the issues, and developed documentation and training for their other facilities. This helped them understand their requirements and scale gradually with the help of lessons learned in the pilot implementation.
But if you think integration ends after installation, then you need to think again. The process of integration actually begins after installation, as you must govern changes and monitor the systems continuously. Additionally, maintaining the systems is also important to keep them in their optimal condition.
Moreover, the healthcare landscape is changing and evolving rapidly with growing technology and new innovations. So, utilizing tools like AI-assisted diagnostics and management tools can make EHR integration much more efficient and effective.
Conclusion
Integrating decades-old legacy systems with modern healthcare systems is not just a technical challenge; it’s an opportunity. By carefully connecting your established systems with modern technologies, you can preserve your workflows and data while taking your practice to modernization.
However, the success of this endeavor depends on assessments, selection of the right technical approach, and careful data management, along with taking the needs of users at heart. But, doing this alone is not feasible; you need an experienced integration partner to bring crucial expertise to navigate complex decisions and technical hurdles.
Want to explore how strategic integration could benefit your organization? Click here to schedule a call with our healthcare IT experts, discuss your unique legacy system challenges, and discover the best ways to modernize your practice.
Frequently Asked Questions
Maintaining integrated legacy systems can be challenging. While they might still function, issues like high maintenance costs, security vulnerabilities, and difficulty integrating with modern tech arise. Reasonably, their lifespan is often limited by these mounting challenges, pushing organizations towards modernization within 5-10 years to remain competitive and secure.
Integrating legacy healthcare systems commonly faces challenges like poor interoperability, security vulnerabilities, high maintenance costs, data silos, and difficulty scaling. Outdated technology often hinders compliance and limits the adoption of modern tools.
For systems without published APIs, direct integration involves methods like:
- Database access: Connecting directly to the system’s database (with caution for data integrity).
- File exchange: Importing/exporting data via files (CSV, XML).
- Robotic Process Automation (RPA): Mimicking human interaction with the UI to extract or input data.
- Middleware/API wrappers: Building custom layers to expose functionality.
Legacy system integration poses risks due to outdated security protocols, unpatched vulnerabilities, and a lack of vendor support. This creates an expanded attack surface, making systems susceptible to modern cyber threats, data breaches, and compliance issues. Compatibility problems also hinder the implementation of modern security tools.
Prioritize legacy system integration based on business criticality, impact on revenue/operations, and technical complexity. Start with systems offering the most immediate value or posing the highest risk if not integrated.
Successful legacy system integration requires strong analytical skills to understand existing architectures, expertise in choosing appropriate integration technologies, like APIs or middleware, robust data migration planning, comprehensive testing, and effective project management. Knowledge transfer and cybersecurity awareness are also crucial.
Maintaining data consistency between legacy and modern systems involves strategies like data synchronization by using batch or real-time, API-led integration, and event-driven architectures. Data governance, validation, and cleansing are also crucial to ensure data accuracy and integrity across hybrid environments.
For legacy integration, essential testing types include integration testing to ensure modules interact correctly, regression testing to prevent new issues, performance testing for system behavior under load, and end-to-end testing to validate entire workflows. Security testing and acceptance testing are also crucial.
Regulatory requirements significantly impact legacy system integration by demanding adherence to data privacy, such as GDPR, HIPAA, and security standards. Older systems often lack these modern features, increasing compliance risks, vulnerabilities, and the complexity and cost of integration due to the need for extensive workarounds and potential legal penalties.
APIs provide a standardized way for old and new systems to communicate. iPaaS platforms offer cloud-based tools and pre-built connectors to streamline and manage integrations. Generative AI and machine learning are emerging to automate code modernization and data mapping. Additionally, containerization (like Kubernetes) allows legacy apps to run in portable environments, and microservices architecture breaks down large legacy systems into manageable, easily integrable components.




