Business Challenges
- Inefficient Manual Claim Processes
- Frequent Claim Denials
- Complex Data Validation
- Scalability Across EHR Platforms
Solution
- Development of an AI-Powered Claim Scrubbing System
- Standardized Claim Scrubbing Across EHRs
- Claim Data Validation and Automation
- Unified Integration Framework
Value Delivered
- Reduced claim denials by 85%, improving revenue cycle efficiency.
- Achieved 60% faster claim submission by automating manual workflows.
- Improved claim data accuracy by 95%, ensuring timely reimbursements.
- Enabled integration with 5+ EHR platforms, ensuring scalability and compliance.
Solution Provided
To address key challenges, we implemented a phased approach leveraging advanced Large Language Model (LLM) technology, carefully integrated with the client’s existing workflows. Building on the successful deployment of the claim scrubbing system, the next step focused on seamless Electronic Health Record integration to improve accessibility and enable real-time data exchange. By utilizing standardized HL7 and FHIR protocols, we ensured compatibility with leading EHR systems, supporting a streamlined and interoperable healthcare data environment.
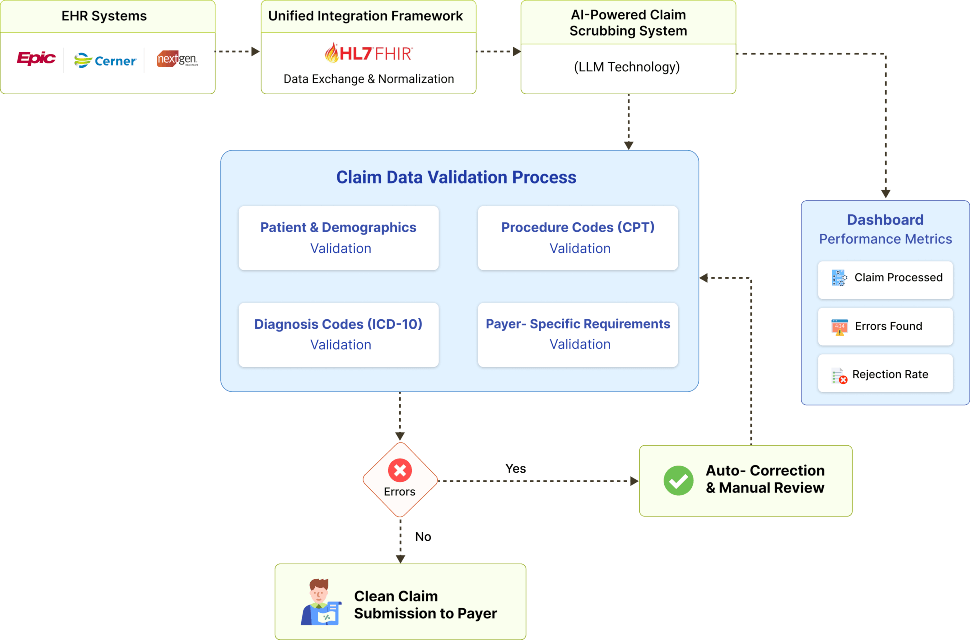
1. Development of an AI-Powered Claim Scrubbing System:
We developed a system powered by LLM technology to analyze claims in real time. The system flagged missing fields, incorrect data, and invalid codes. It provided actionable recommendations and automatic corrections based on payer guidelines, improving accuracy and reducing human effort.
- LLM models trained on historical claims to replicate staff expertise.
- Error detection based on payer-specific rules and policies.
- Automated corrections for common errors to minimize manual intervention.
- Dashboard for billing staff to review flagged claims.
2. Claim Data Validation and Automation:
The system is integrated directly with EHRs to fetch patient data, validate claim details, and flag errors. Automated checks were performed for missing demographic information, incorrect procedure codes, and payer-specific compliance requirements.
- Automated claim validation using payer-specific rules fetched from integrated EHRs.
- Real-time flagging of errors and missing information.
- Ensured compliance with ICD-10, CPT, and payer-specific coding standards.
- Improved accuracy and reduced manual rework for billing staff.
3. Customizable Error Validation Framework:
The system employed a modular validation framework to identify discrepancies in procedure codes (CPT), diagnosis codes (ICD), and insurance details. It provided detailed explanations for errors and ensured compliance with payer-specific requirements.
- Support for custom validation rules based on client workflows.
- Real-time feedback to ensure data accuracy before submission.
4. Unified Integration Framework:
We developed a robust middleware that serves as a bridge between the claim scrubbing system and various EHR platforms, ensuring seamless and secure data exchange. The framework leverages industry-standard HL7 and FHIR protocols to enable standardized communication while incorporating custom adapters to integrate proprietary EHR APIs such as Epic, Cerner, and NextGen. This middleware automates claim data retrieval and updates in real time, eliminating the need for repetitive manual configurations. Its modular design supports easy scalability, allowing quick integration with additional EHR systems in the future.
- Middleware acts as a bridge for seamless EHR communication.
- Utilizes HL7 and FHIR for standardized data exchange.
- Custom adapters for proprietary EHRs like Epic, Cerner, and NextGen.
- Modular design ensures scalability for future EHR integrations.
Business Value
Improving UX
Helped being on the same page with the patients. We improved User experience and made the accuracy of the results higher.
Developing All Flow
Helped in having a competitive advantage. We chose a proper tech stack, developed all flow from A to Z and implemented in real life.
Optimization
Increasing operational speed by 2 times. Now all data in one place. Increasing operational speed by 2 times. Now all data in one place.
Transform Your Business with Powerful Insights Enabled by Cutting- Edge Generative AI