Chronic Care Management CMS Guidelines & Reimbursement

Chronic Care Management (CCM) is an integral part of healthcare. Basically, its purpose is to improve the health and well-being of people with chronic illnesses. This can help to enhance their quality of life. Healthcare professionals provide CCM services.
These services not only include creating and managing care plans, and coordinating care between providers but also support patients and their families.
CMS has established Current Procedural Terminology (CPT) codes to reimburse providers for their CCM services.
From the beginning of January 2015, medicare started paying physicians for Chronic care management (CCM) services using multiple CPT codes. Those services are for Medicare patients having a minimum of two or more chronic conditions.
Reimbursement can be provided according to CMS rules and guidelines. This then ensures a better quality of care and lowers the risk of complications in patient health and hospital readmissions.
Providers can earn monthly recurring revenue better when they provide Chronic Care Management services. This also reduces their staff requirements and office expenses. Please continue reading this post to learn more about the Chronic care management CPT codes and billing process in detail.
CMS Guidelines for Chronic Care Management:
CMS has introduced some guidelines to get benefits of reimbursement for chronic care management services. Both patients and providers must follow those guidelines strictly to get more reimbursement.
Patient & Provider Guidelines for Chronic Care Management Program
Free Guide DownloadFollowing are some criteria for patients and providers.
Eligible patients to avail benefits of CCM:
- Patients with at least two long-term chronic diseases are predicted to persist for at least a year.
- Chronic conditions may have a significant risk of patient death or serious harm to patient health.
- Patients who are Medicare Part B beneficiaries then those patients can be eligible for chronic care management services.
Examples of complex chronic conditions that may require CCM services include, but are not limited to:
- Chronic heart failure
- Chronic obstructive pulmonary disease (COPD)
- Diabetes
- Chronic kidney disease
- Cancer
- Dementia or other cognitive impairment
- Chronic pain syndromes
- HIV/AIDS
Who can bill CCM services:
Both physician practitioners and non-physician practitioners can bill for Chronic Care management services.
Primarily they include:-
- Physicians and physician assistant
- Certified Nurse practitioners
- Nurse Midwives
- Clinical specialist nurse practitioners
- Clinical nursing staff
Non-practitioner Clinical staff may also provide CCM services under the guidance of practitioner physicians. In this case, only practitioners and physicians can bill for CCM services.
Two healthcare physician practitioners can also provide CCM services to patients. However, only one physician can bill for these services in one month.
Acceptance of consent for CCM services from the patient:
Firstly, the provider must obtain consent from the patient to receive reimbursement for CCM services provided. This then creates a mutual agreement between the patient and the provider.
CMS does not impose a standard format for patient consent during CCM services. However, the consent must include the patient’s agreement to the following:
- Authorization to use patient medical information and share it for patient evaluation to provide better care.
- Awareness about CCM services and required cost sharing as a Co-pay
- Patients can stop CCM services at any time, at the end of running calendar month
- Only one provider can bill for CCM services during a single calendar month
- Privacy Consent to call, text, and email.
Services that can be billed under CCM
- Non-face-to-face consultation.
- Managing patient health records and storing them in a certified EHR.
- Patient care management includes assessing the patient’s medical, functional, and psychosocial needs.
- Creating a personalized patient-centric care plan and assigning it to the patient electronically as a part of care.
- Seamless transitions of care, referral, and follow-up care of patients using various technologies.
- Reviewing the patient care plan and progress and updating the care plan if required.
- Access to patient care 24/7 in any emergency.
- Multiple ways of communication can be adopted, like phone calls, text messages, and emailing.
- Formation of a team of qualified healthcare professionals to ensure better patient care.
- Continuity of care is essential. This can be achieved by coordinating and communicating with other providers involved in the patient’s care. These providers may include primary care physicians, specialists, and caregivers.
What Are CPT Codes And Reimbursement Rates For Chronic Care Management?
What are CPT Codes?
CPT codes are standardized to describe medical, surgical, and diagnostic services healthcare professionals provide. The American Medical Association (AMA) maintains codes that insurance companies use to determine reimbursement rates. This includes Medicare and Medicaid. These codes cover healthcare services.
How Does CCM CPT Codes And Billing Works
CPT code 99490 refers to non-face-to-face care management services.
It is used to bill for an initial 20 minutes or more of services provided by clinical staff. These codes are as follows:
CMS has divided CCM services and billing CPT codes into two categories: Non-Complex Chronic and Complex Chronic Conditions.
Let’s discuss them in detail.
CPT codes for Non-Complex Chronic Conditions
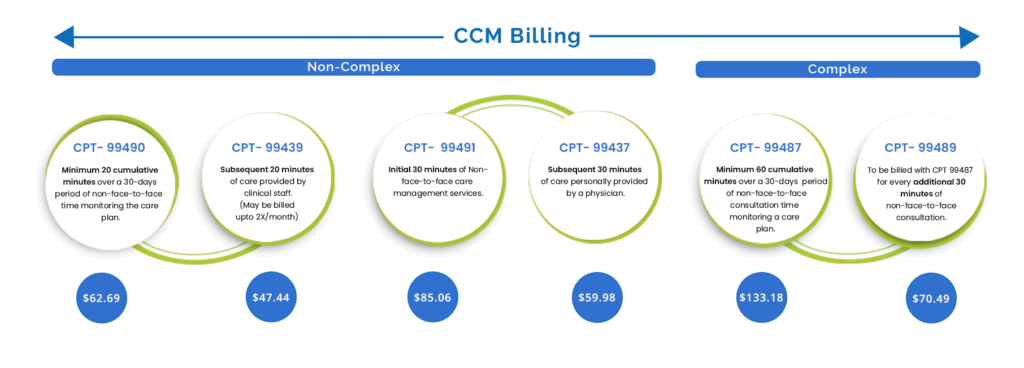
Non-complex chronic conditions are stable and well-controlled and have few complications or difficulties. Although, people with non-complex chronic diseases often need routine care and monitoring. Additionally, medication management is necessary. However, their health state stays the same and does not change unexpectedly. Following are the codes to bill non-complex CCM services:
CPT code 99490:
CPT code 99490 is used for billing. It covers initial care management services that last 20 minutes or more but are not face-to-face. These services must be provided by clinical staff. Moreover, this is provided to patients with two or more chronic conditions.
The services may include the following:
- Communication with the patient and/or their caregiver
- Coordination of care with other providers
- Care plan review and updating
- Medication management
- Other related activities.
Providers can bill these CPT codes once a calendar month. The Average reimbursement rate for the code is approximately $ 64.
CPT code 99491:
This code applies to the initial 30 minutes of non-face-to-face care management services. However, only qualified physician practitioners must provide these services. Providers can bill this code multiple times in a month in addition to 99491. The average monthly reimbursement for this code is approximately $86.
CPT code 99439:
This code is used for the next 20 mins CCM services provided by clinical staff in addition to CPT code 99490. Providers can bill this code twice a month in addition to 99490. The average reimbursement for this code is approximately $48 per month.
CPT code 99437:
This code is used for the next 30 mins CCM services provided by clinical staff in addition to CPT code 99491. The provider is not limited to billing this code as it is necessary. The average reimbursement for this code is approximately $41 per month.
CPT codes for Complex Chronic Conditions
Complex chronic illnesses are health conditions that require a lot of effort to manage. This includes medical decisions, care coordination, and management of the patient. Following are the examples of “these conditions”:
- Many chronic conditions
- Severe and uncontrolled chronic conditions
- Chronic conditions with complications
- Conditions requiring frequent changes in care plans.
CPT code 99487
Clinical staff must spend at least 60 minutes monthly on CCM services. These services also involve moderate to high medical decision-making complexity. These include the following:
- Managing medication regimens for multiple chronic conditions.
- Coordinating care among multiple providers.
- Addressing multiple comorbidities or complications.
- Addressing the social determinants of health that impact the patient’s care.
Providers can bill these CPT codes once a calendar month. The average reimbursement for this code is approximately $134 per month.
CPT code 99489:
Providers must complete an additional 30 mins CCM services in addition to the initial 60 mins complex CCM services. Moreover, this code can be billed repeatedly in a single calendar month. The average reimbursement for the code is approximately $ 70 per month.
How to Bill Chronic Care Management?
To bill Chronic care management services, the provider must submit the claim through CMS. Below are some key elements that should be included in a claim while submitting:
- Patient details
- Patient enrolment details with consent
- Patient clinical details with chronic disease and ICD codes
- Patient insurance
- Provider details with valid NPI and account details
- Date and place of services
- Qualified CPT codes
- Running care plan with progress and updations
- Cumulative time logged by clinical staff and physicians
Steps to Submit Claim:
- Before submitting the bill or claim for CCM services, ensure all CMS guidelines have been followed for each patient.
- Submit a claim by entering above explained details
- Send invoice to the patient if any co-pay is applicable
- Correct the claim if any denial occurs.
Conclusion
In conclusion, understanding the Chronic Care Management (CCM) guidelines and reimbursement processes is crucial for healthcare providers seeking to enhance patient care while maximizing revenue. By following CMS guidelines and utilizing CPT codes, providers can offer comprehensive non-face-to-face care management services to patients with chronic conditions. It improves patients’ quality of life and contributes to a sustainable revenue stream for healthcare practices. Embracing CCM is not just a financial opportunity; it’s a commitment to delivering better, more coordinated care to those who need it most.





Just wish to say your article is as astonishing. The clarity in your post is just great and i can assume you are an expert on this subject. Fine with your permission let me to grab your feed to keep updated with forthcoming post. Thanks a million and please continue the rewarding work.