Business Challenges
- Complex Multi-Specialty Coding Requirements
- High Denial Rates & Manual Rework
- Inefficient Prior Authorization Management
- Fragmented Billing Workflows
- Compliance & Audit Concerns
- Resource Allocation Inefficiencies
Solution
- Intelligent Medical Coding Automation: AI agents automatically assign CPT, ICD-10, and HCPCS codes with 98% accuracy.
- Predictive Denial Management: Machine learning models identify denial risks before submission and implement corrective actions.
- Automated Prior Authorization Workflows: AI-powered system reduces approval times from 72 hours to 4 hours.
- Unified RCM Data Platform: Real-time visibility into coding, billing, and collection metrics across all locations.
- Intelligent Compliance Monitoring: Continuous AI-powered audit preparation and compliance verification.
- Smart Resource Optimization: AI handles routine tasks while routing complex cases to specialists.
Value Delivered
- 37% reduction in days in A/R from 45 to 28 days, improving cash flow.
- 60% decrease in initial denial rates from 30% to 12%, saving 180 hours monthly.
- $2.3 million annual revenue recovery through automated denial management.
- 98% coding accuracy rate compared to 87% manual baseline.
- $480,000 annual labor cost savings by eliminating 6 FTE positions.
- 65% reduction in patient complaints through faster processing.
Solution Implementation
Our client, a rapidly expanding multi-specialty outpatient network with 12 practices across three states, faced critical challenges in managing their revenue cycle operations. With over 200 providers across mental health, physical therapy, wound care, orthopedics, and primary care, they struggled with inconsistent coding practices, high denial rates, and inefficient workflows that were hampering their ability to scale effectively. The organization was losing approximately $200,000 monthly to preventable denials and experiencing significant cash flow delays due to manual processes that couldn't keep pace with their growth trajectory.
Recognizing the need for a comprehensive transformation, we implemented an AI medical software that revolutionized their entire revenue cycle operation. Our solution integrated seamlessly with their existing EHR system and created an intelligent workflow that could handle the complexity of multi-specialty coding while maintaining the accuracy and compliance standards required for their diverse patient population.
Intelligent Medical Coding Automation
The foundation of our solution is centered on deploying AI agents capable of processing clinical documentation across all specialties with remarkable precision. These intelligent systems analyze physician notes, lab results, diagnostic reports, and procedure documentation to automatically assign the most appropriate codes, while considering specialty-specific requirements and payer preferences.
The AI coding platform integrated seamlessly with existing EHR workflows, eliminating the need for manual code lookup and verification processes that previously consumed hours on a daily basis. Advanced natural language processing capabilities enabled the system to interpret complex clinical narratives and translate them into accurate billing codes, while machine learning algorithms continuously improve accuracy based on coding patterns and feedback from certified coders.
- Specialty-Specific Intelligence: AI models trained on wound care procedures automatically differentiate between diagnostic and interventional treatments
- Real-Time Validation: The system performs immediate code validation against payer policies and medical necessity requirements.
- Continuous Learning: Machine learning capabilities adapt to new coding guidelines and payer policy changes without manual reprogramming.
- Quality Assurance Integration: Built-in quality checks ensure coding accuracy while flagging cases requiring human review.
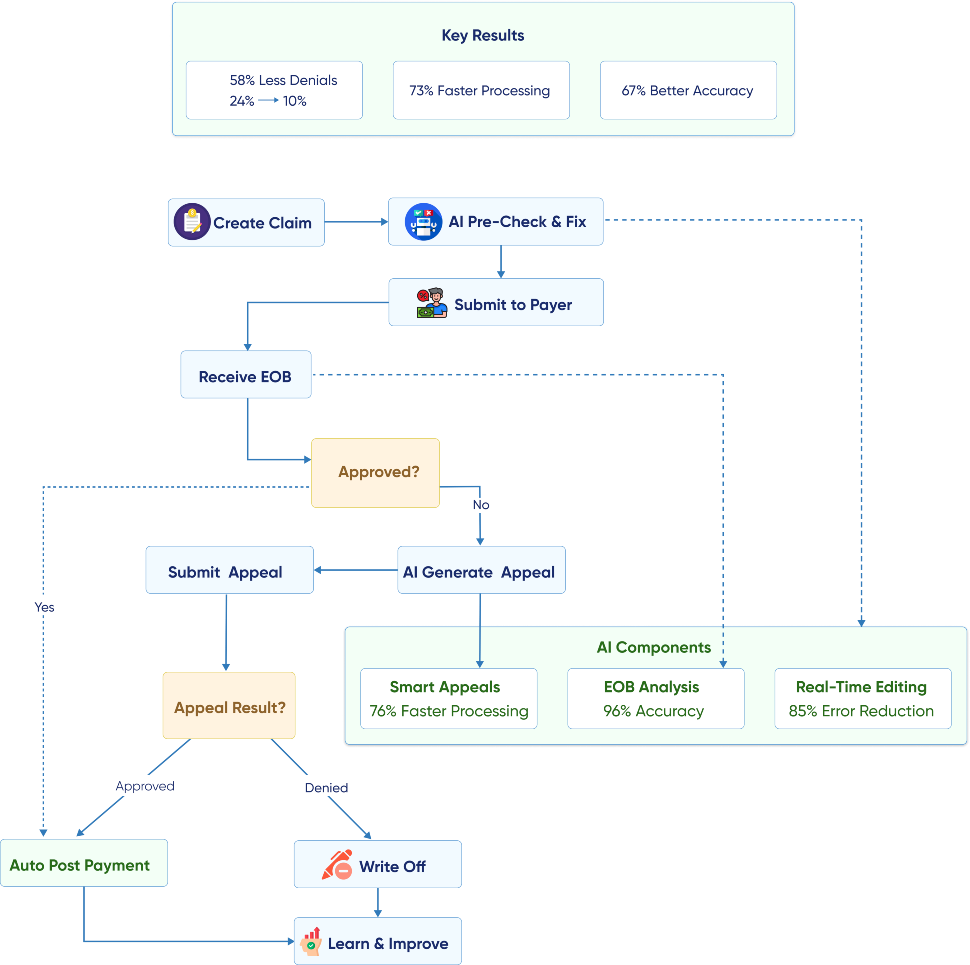
Predictive Denial Management
Our AI-powered denial prevention system transformed the client's approach to claims management by identifying and addressing potential issues before they result in denials. The system analyzes historical denial patterns, payer behavior, and claim characteristics to predict denial probability with 94% accuracy.
Machine learning algorithms continuously evaluate thousands of data points, including diagnosis codes, procedure codes, patient demographics, insurance coverage details, and historical payer responses to create comprehensive risk profiles for each claim. The platform maintains real-time connectivity with major payer systems to validate coverage and benefits information, ensuring claims are submitted with complete and accurate supporting documentation that meets specific payer requirements.
- Pre-Submission Optimization: AI agents automatically review claims for common denial triggers and correct issues before submission.
- Intelligent Appeals Management: The system automatically generates appeals with appropriate supporting documentation within 2 days.
- Payer-Specific Intelligence: Machine learning models identify patterns in payer behavior and adjust claim formatting accordingly.
- Performance Monitoring: Real-time analytics provide immediate visibility into denial trends for proactive adjustments.
Automated Prior Authorization Workflows
The prior authorization automation system eliminated one of the most time-consuming aspects of RCM operations while dramatically improving patient satisfaction. Our AI agents manage the entire prior authorization lifecycle, from initial submission through approval tracking and renewal management.
The system also maintains comprehensive databases of payer-specific prior authorization requirements, automatically determining which procedures require approval based on patient insurance coverage and clinical indications. Advanced workflow automation handles all communication touchpoints with payers, including initial submissions, status inquiries, and follow-up requests, while providing real-time updates to clinical staff and patients throughout the authorization process. Integration with scheduling systems enables automatic appointment confirmation once authorizations are received, streamlining the entire patient care pathway.
- Intelligent Submission: AI systems automatically determine prior authorization requirements based on procedure codes and patient insurance.
- Automated Follow-Up: The system manages all payer communication and escalates cases requiring human intervention.
- Real-Time Status Updates: Providers and patients receive immediate notifications when authorizations are approved.
- Renewal Management: AI agents automatically track expiration dates and initiate renewal processes.
Unified RCM Data Platform
Our integrated platform provides comprehensive visibility into RCM performance across all locations and specialties, enabling data-driven decision making and continuous optimization. The system consolidates information from multiple sources into a single, actionable dashboard that RCM directors can use to monitor performance and identify opportunities for improvement. Advanced analytics capabilities process millions of data points daily to generate insights on coding patterns, collection trends, payer performance, and operational efficiency metrics. The platform's predictive analytics engine identifies potential revenue leakage points and recommends corrective actions before they impact financial performance. Customizable reporting features allow stakeholders at all levels to access relevant metrics and KPIs tailored to their specific roles and responsibilities within the revenue cycle operation.
- Real-Time Analytics: Live dashboards display key performance indicators across all locations and specialties.
- Predictive Insights: Machine learning algorithms identify trends that might impact future performance.
- Automated Reporting The system generates comprehensive reports, eliminating manual report preparation.
- Performance Benchmarking: Built-in benchmarking capabilities to compare performance across locations and time periods.
Business Value
Improving UX
Helped being on the same page with the patients. We improved User experience and made the accuracy of the results higher.
Developing All Flow
Helped in having a competitive advantage. We chose a proper tech stack, developed all flow from A to Z and implemented in real life.
Optimization
Increasing operational speed by 2 times. Now all data in one place. Increasing operational speed by 2 times. Now all data in one place.
Transform Your Business with Powerful Insights Enabled by Cutting- Edge Generative AI



















