Business Challenges
- Undetected Revenue Loss Across Claims
- Manual Billing Review Inefficiencie
- Complex Prior Authorization Delays
- Inconsistent Charge Capture Processes
- High Claim Denial and Rejection Rates
- Resource-Intensive Appeals Management
- Limited Revenue Performance Visibility
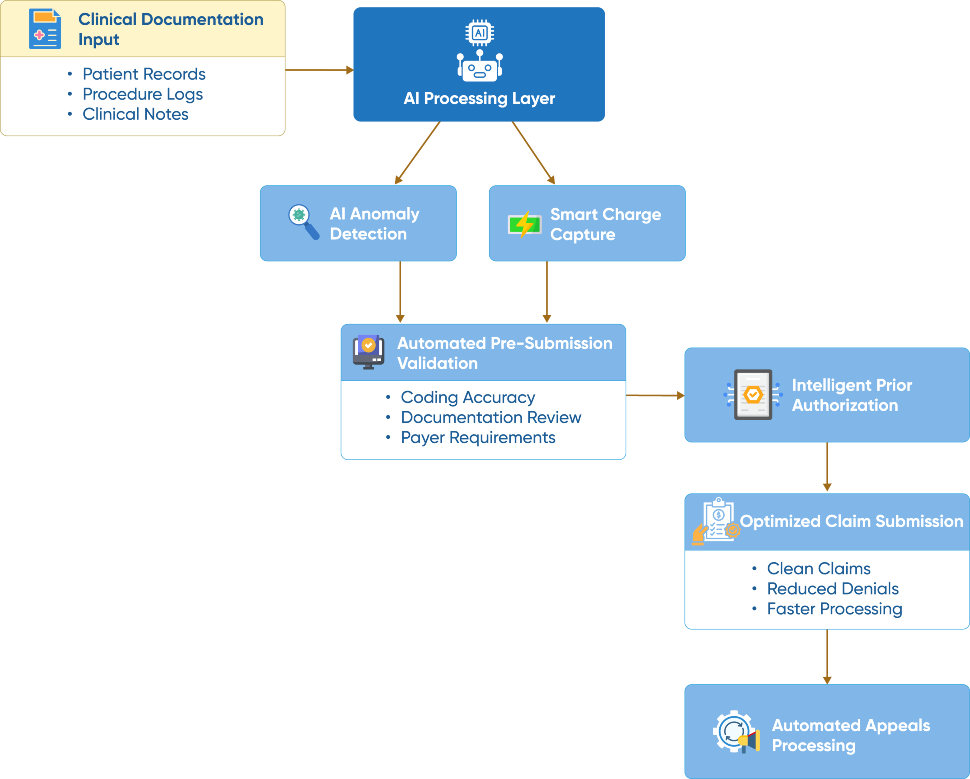
Solution
- AI-Powered Anomaly Detection Engine
- Automated Pre-Submission Billing Validation
- Intelligent Prior Authorization Workflow
- Smart Charge Capture Optimization
- Predictive Denial Prevention System
- Automated Appeals Processing Framework
Value Delivered
- AI detection identifies 95% of potential revenue leaks, preventing $2.3M annual losses across the client portfolio.
- Automated validation reduces manual review time by 65%, allowing staff to focus on complex billing scenarios.
- Intelligent workflow accelerates prior authorization approvals by 40%, reducing treatment delays and improving cash flow.
- Smart optimization increases charge capture accuracy by 85%, maximizing revenue from every patient encounter.
- Predictive system reduces claim denials by 42%, improving first-pass resolution rates and reducing rework.
- Automated processing handles 78% of appeals without human intervention, reducing administrative costs by $450K annually.
Solution Implementation
Our client, a leading RCM vendor serving 150+ healthcare facilities across California, was experiencing significant revenue loss due to manual billing processes and inconsistent quality controls. Their team of 45 billing specialists was overwhelmed by the complexity of modern healthcare billing, resulting in missed charges, delayed submissions, and high denial rates that impacted both their reputation and client retention. The organization needed an intelligent solution that could scale with their growing client base while maintaining the highest standards of billing accuracy and compliance. Our AI-enhanced billing review tool provided a comprehensive automation platform that transformed their entire revenue cycle operation from reactive problem-solving to proactive revenue optimization.
AI-Powered Anomaly Detection Engine
Our advanced AI healthcare solutions continuously monitors billing patterns, charge relationships, and reimbursement trends to identify potential revenue loss before it impacts cash flow. The engine uses machine learning algorithms trained on millions of healthcare transactions to recognize subtle patterns that indicate underbilling, missed charges, or coding inconsistencies. This proactive approach enables RCM teams to address revenue optimization opportunities in real-time rather than discovering losses weeks or months after the fact. The system integrates seamlessly with existing billing workflows and provides actionable insights that help teams prioritize their efforts on the highest-impact revenue recovery opportunities while maintaining operational efficiency.
- AI monitors billing patterns to identify revenue loss in real-time.
- Machine learning recognizes subtle underbilling and missed charge patterns.
- Proactive alerts enable immediate correction before revenue impact.
- Actionable insights prioritize the highest-impact revenue recovery opportunities.
Automated Pre-Submission Billing Validation
The AI system performs comprehensive validation checks on every claim before submission, analyzing coding accuracy, documentation completeness, and payer-specific requirements to ensure optimal reimbursement potential. This automated validation process eliminates common billing errors that lead to denials and delays while ensuring compliance with constantly changing payer policies and regulations. The system maintains an extensive database of payer rules, coverage policies, and billing guidelines that is updated in real-time to reflect the latest requirements. Advanced validation algorithms check for coding conflicts, medical necessity support, and proper modifier usage to maximize clean claim rates and accelerate reimbursement cycles.
- Comprehensive validation checks ensure optimal reimbursement potential.
- Automated process eliminates common billing errors and compliance issues.
- Real-time payer rule updates maintain current compliance standards.
- Advanced algorithms maximize clean claim rates and accelerate payments.
Intelligent Prior Authorization Workflow
Our AI system streamlines the prior authorization process by automatically identifying procedures that require approval, gathering necessary documentation, and submitting requests through the most efficient channels available. The intelligent workflow system tracks authorization status in real-time and provides automated follow-up when approvals are delayed or additional information is required. Machine learning algorithms analyze historical authorization patterns to predict approval likelihood and suggest alternative approaches when denials are anticipated. This comprehensive automation reduces the administrative burden on clinical and billing staff while ensuring that necessary approvals are obtained quickly to prevent treatment delays and revenue disruption.
- Automatically identifies procedures requiring authorization and gathers documentation.
- Real-time tracking and automated follow-up accelerate approval processes.
- Machine learning predicts approval likelihood and suggests alternatives.
- Comprehensive automation reduces administrative burden and prevents delays.
Smart Charge Capture Optimization
The AI system analyzes clinical documentation, procedure logs, and billing patterns to identify missed charges and optimize revenue capture across all service lines. Advanced natural language processing capabilities review clinical notes, operative reports, and ancillary service documentation to ensure that all billable activities are properly captured and coded. The system provides real-time feedback to clinical staff about documentation requirements and suggests additional charges based on documented care activities. Continuous learning algorithms adapt to specific practice patterns and specialties to improve charge capture accuracy over time while maintaining compliance with billing regulations and medical necessity requirements.
- Advanced NLP reviews clinical documentation for missed charge identification.
- Real-time feedback improves documentation and suggests additional charges.
- Continuous learning adapts to practice patterns for improved accuracy.
- Compliance monitoring ensures adherence to billing regulations and requirements.
Business Value
Improving UX
Helped being on the same page with the patients. We improved User experience and made the accuracy of the results higher.
Developing All Flow
Helped in having a competitive advantage. We chose a proper tech stack, developed all flow from A to Z and implemented in real life.
Optimization
Increasing operational speed by 2 times. Now all data in one place. Increasing operational speed by 2 times. Now all data in one place.
Transform Your Business with Powerful Insights Enabled by Cutting- Edge Generative AI



















