"Our intake process used to overwhelm both staff and patients, with forms everywhere, long wait times, and missing information. Thinkitive digitized everything, allowing new patients to be onboarded in minutes. It’s made a huge difference in patient comfort and first impressions."
Feature-Rich Custom Primary Care EHR Solutions Specific to Your Practice
Empower your primary care practice with custom primary care EHR development with specific features aligned with your clinical workflows and administrative needs.
CLIENT TESTIMONIALS
What Our Clients Have to Say About Thinkitive’s EHR Development for Primary Care
Discover our latest ventures in primary care software development for our clients. Learn about their unique challenges and prepositions and how we helped them streamline their practice with custom healthcare software solutions.
Pre-Built Components to Accelerate EHR Development Timeline Primary Care
Develop EHR with patient portal primary care, and other specific features and functionalities faster with Thinktive’s pre-built primary care EMR software development components.
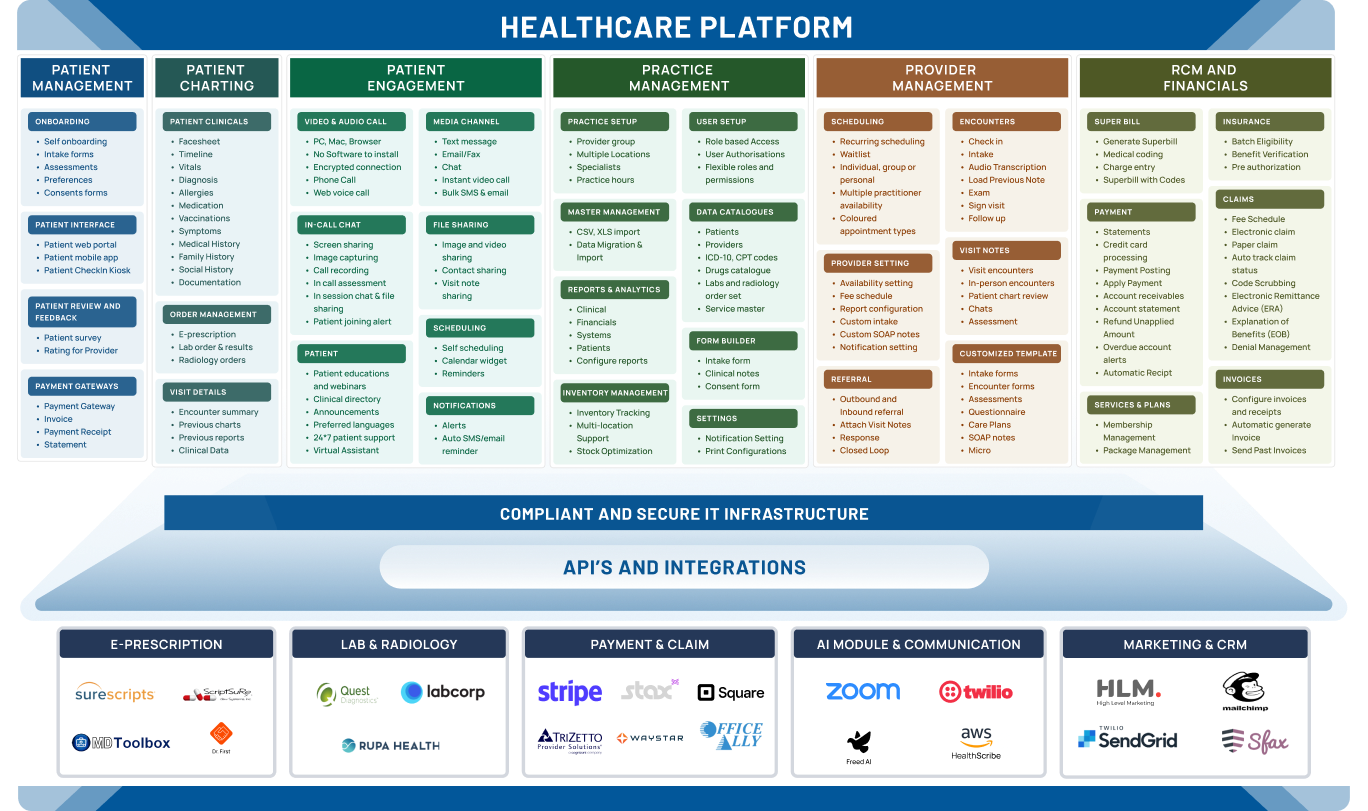
Comprehensive Connectivity with All-in-One EHR System Integrations
Seamless connectivity with custom EHR integration with ePrescribing, labs, billing and patient engagement system.
ePrescription & Labs Integration
We provide affordable primary care EHR development with ... ePrescriptions and Labs integration to enable you to send orders directly from the EMR system. These integrations offer multiple benefits, from reducing errors to improving clinical efficiency and reducing the overall cost of care for both patients and providers.

Surescripts
Surescripts is the leading e-prescribing network that helps in improving medication ... safety and convenience for patients, providers, pharmacies, and payers. Integrate Surescripts during primary care EHR software development, enabling secure electronic e-prescribing and real-time access to patient medication history.
Billing & Payment
Safe, secure, and seamless healthcare transactions with our billing, ... payment, and point-of-sale integrations into your primary care EHR. Give your virtual care practice a comprehensive real-life healthcare ecosystem with EHR development company for primary care clinics.

Waystar
Waystar provides healthcare revenue cycle management solutions. Integrating it ehr development for primary care streamlines claims processing, reduces denials, and optimizes revenue capture through automation and AI, improving financial efficiency for healthcare organizations.
Communication
Facilitate real-time communication with patients via various ... media with integrated patient portal development for primary care EHR. Give your virtual care practice a comprehensive real-life healthcare ecosystem.

Sfax
Sfax is a secure faxing solution designed for healthcare. Integrating it EHR development for primary care to enable secure exchange of patient information like faxes within the system, ensuring patient data privacy and compliance with HIPAA regulations. This streamlines communication and protects sensitive medical information.

Calculate Your Primary Care EHR Development Cost & ROI in 2 Minutes
Discover primary care EHR development cost and its return on investment. Our calculator is based on real data from 500+ implementations.
From Discovery to Deployment in 12-16 weeks
We have grown a niche EMR EHR software development to curate an ideal EMR EHR software solution for your unique needs.
1-2 Weeks
Start by understanding your practice’s unique workflows and requirements.
- Stakeholder interviews and collaborative workshops
- Audit of current systems and infrastructure
- End-to-end workflow mapping and documentation
- Success criteria definition based on clinical priorities
Key Deliverables
- Feature Requirement Document
- Stakeholder Analysis Report
- Current State Assessment
- Gap Analysis Report
Resource Allocation
- 2 Business Associates
- 5 Full-Stack Developers
- 2 UX Designers
- 1 QA Engineer
2-3 Weeks
Collaborate to transform insights into intuitive, role-based, and user-friendly EHR workflows and interfaces.
- Wireframing key user journeys (charting, scheduling, documentation)
- Prototyping clinical and admin modules
- Designing specialty-specific dashboards and navigation
- Conducting feedback loops with end users
Key Deliverables
- Workflow-Based Wireframes
- Clickable Prototype
- UI Style Guide & Component Library
- User Feedback Summary
Resource Allocation
- 2 UX Designers
- 1 UI Designer
- 2 Business Associates
- 1 Technical Architect
8-12 Weeks
Build custom, secure, and precise EHR modules based on your requirements.
- Backend and frontend module development
- Role-based access control and user management
- Specialty-specific templates (e.g., SOAP, PHQ-9, HPI)
- Automated coding, alerts, and decision logic
- Sprint-based testing and QA cycles
Key Deliverables
- Fully Developed Frontend & Backend Modules
- Clinical Templates & Configurations
- Access Control Setup
- Unit & Integration Test Reports
Resource Allocation
- 5 Full-Stack Developers
- 2 QA Engineers
- 1 DevOps Engineer
- 1 Project Manager
2-3 Weeks
Integrate your EHR with labs, pharmacies, and billing platforms.
- Integration with labs (e.g., LabCorp, Quest)
- eRx and pharmacy integration via SureScripts
- Clearinghouse or RCM platform connectivity
- HL7/FHIR interface development
- Integration testing with real data
Key Deliverables
- Integrated API Endpoints
- Lab & Pharmacy Connectivity Setup
- Interface Engine Configuration
- Integration Test Reports
Resource Allocation
- 2 Integration Specialists
- 2 Backend Developers
- 1 QA Engineer
- 1 Project Manager
1-2 Weeks
Ensuring your EHR meets all regulatory and data protection standards, including HIPAA.
- HIPAA security and privacy compliance review
- Role-based access and audit trail validation
- ONC-Certification alignment (if required)
- Risk assessments and documentation
- Encryption and secure data handling protocols
Key Deliverables
- Compliance Checklist & Audit Report
- Risk Assessment Summary
- Data Protection Policy Documentation
- Role-Based Access Validation Report
Resource Allocation
- 1 Compliance Officer
- 1 Security Specialist
- 1 QA Engineer
- 1 Technical Lead
2-3 Weeks
Continuous support for a seamless EHR rollout, from provider training to data migration.
- Final UAT (User Acceptance Testing)
- Staff training and onboarding
- Legacy data migration
- Production deployment and monitoring
- Post-go-live bug fixes and enhancements
Key Deliverables
- Production-Ready EHR System
- Training Materials & Sessions
- Go-Live Checklist & Rollout Plan
- SLA-Based Support Plan
Resource Allocation
- 2 Support Engineers
- 1 Project Manager
- 1 QA Lead
- 1 Training Specialist
Real Stories of Primary Care Practices Thriving with Custom EHRs
Discover how multiple providers moved from one-size-fits-all systems to custom EHRs that streamline care and boost patient outcomes.
Built to Meet Every Healthcare Standard
The foundation of healthcare data security and privacy
HIPAA Compliance
Protect patient health information by adhering to strict privacy and security safeguards.
Fines & Penalties
- Tier 1: Unaware of violation — $141 to $71,162 per violation
- Tier 2: Reasonable cause (not willful) — $1,424 to $71,162 per violation
- Tier 3: Willful neglect, corrected — $14,232 to $71,162 per violation
- Tier 4: Willful neglect, not corrected — $71,162 to $2,134,831 per violation
- Annual Maximum: $1.5M (Per Violation Type)
Why It’s Required
- Expands and strengthens HIPAA enforcement
- Requires breach notification to patients and HHS
- Promotes secure EHR adoption and meaningful use
- Enables State Attorneys General to file HIPAA lawsuits
- Boosts patient confidence in digital health systems
Process
- Conduct EHR system audits for compliance gaps
- Encrypt all stored and transmitted ePHI
- Establish breach detection and reporting procedures
- Train staff on HITECH-specific privacy/security updates
- Maintain detailed documentation for audit readiness
Our HIPAA Compliance Partners
ONC Certification
Ensures that your EHR meets federal standards for safety, usability, and interoperability.
Non-Compliance Risks
- Using uncertified EHR systems - Ineligible for CMS incentives (MIPS, Medicaid PI)
- Certification non-compliance - Subject to CMS payment adjustments or scoring penalties
- Vendor decertification - Removal from CHPL and reduced provider trust
- Repeat violations or program exclusion - Long-term loss of eligibility and reputational harm
Why It’s Required
- Required for participation in federal incentive programs (like Promoting Interoperability)
- Required for participation in federal incentive programs (like Promoting Interoperability)
- Demonstrates compliance with national standards for security and interoperability
- Enhances trust among providers, payers, and patients
- Enables seamless data exchange between providers and health systems
- Protects your reputation by aligning with a federally approved certification
Process
- Choose an EHR system certified under the ONC Health IT Certification Program
- Ensure compliance with 2015 Edition Cures Update criteria (including FHIR APIs)
- Verify support for clinical quality measures and interoperability standards
- Implement Real World Testing and attestations as required
- Partner with a vendor experienced in certified EHR development and maintenance
Our Partners
FHIR/HL7
The modern backbone of real-time, interoperable healthcare data exchange.
Non-Adhrence Risks
- Poor compatibility with apps and systems
- Integration breakdowns and data silos
- Non-compliance with CMS/ONC rules
- Regulatory attention and data blocking risks
- No readiness for AI, remote care, or digital growth
Why It’s Required
- Required under CMS and ONC Interoperability mandates
- Enables seamless data exchange between systems, payers, and patient-facing apps
- Future-proofs your EHR system for upcoming regulations and digital health innovation
- Enhances patient access to data via standardized APIs
- Supports integration with 3rd-party tools, remote monitoring, and care coordination apps
Implementation Process
- Adopt FHIR-based APIs as per ONC 2015 Cures Update criteria
- Map clinical and administrative data to FHIR resource models
- Ensure secure authentication (e.g., SMART on FHIR, OAuth 2.0)
- Test interoperability with external systems, apps, and payers
- Monitor compliance with CMS and ONC guidelines around data exchange and access
Our FHIR-HL7 Compliance Partners
21st Century Cures Act
Empowers patients with data access and drives interoperability across systems.
Fines & Penalties
- Up to $1M per violation for developers, HIEs, and HINs engaged in information blocking
- Loss of CMS incentives for non-compliant providers
- Zero score in MIPS Promoting Interoperability category
- Reduced Medicare payments to hospitals and CAHs
- Exclusion from ACO participation for at least one year
Why It Matters
- Mandated by ONC and CMS for patient access to records
- Drives transparency and patient-centered care
- Requires seamless API access to health information
- Enables compliance with FHIR and SMART on FHIR standards
- Essential for future CMS reimbursement and program eligibility
Implementation Steps
- Enable API-based access to EHR data as per Cures Act Final Rule
- Prevent information blocking through clear data-sharing policies
- Adopt certified EHR technology that meets ONC 2015 Cures Update
- Train staff on permissible exceptions and patient data rights
- Monitor compliance, patient access logs, and information requests
Our 21st Century Cures Act Compliance Partners
Medical Coding Standards
Standardizes clinical language to ensure accurate billing, reporting, and care.
Non-Compliance Consequences
- Claim denials or delays due to incorrect CPT/ICD codes>
- Revenue loss - reimbursement underpayments and recoupments
- Audit exposure from CMS or payers triggered by miscoding
- False Claims Act liability for upcoding, unbundling, or misrepresenting services
- Exclusion from Medicare/Medicaid for persistent violations of NCCI or coding rules
Advantages
- Ensures accurate medical billing and prevents claim denials
- Supports timely reimbursements from insurers and CMS
- Reduces risk of fraud investigations and legal exposure
- Maintains payer trust and long-term contract eligibility
- Enables compliance with national coding updates (e.g., CMS, AMA)
Process
- Implement automated coding validation tools
- Stay aligned with CMS and AMA coding updates
- Regular internal audits and coding reviews
- Train staff on evolving coding standards and edits (e.g., NCCI)
- Integrate intelligent prompts into EHR for real-time support
Our Medical Coding Standards Adherence Partners
SOC 2 Type II
Validates your system’s operational security, availability, and data integrity controls.
SOC 2 Non-Certification Risks
- Loss of business contracts due to security concerns
- Reputational damage from failed audits or data breaches
- Potential legal exposure in breach-related lawsuit
- Operational disruptions due to system downtime
- Reduced partner and payer confidence in your platform
Why It Matters?
- Demonstrates commitment to data security & integrity
- Builds trust with healthcare providers and partners
- Ensures safe handling of PHI and ePHI in cloud environments
- Strengthens resilience against breaches & system failures
- Aligns with HIPAA and industry-recognized security standards
Process We Follow
- Conduct annual third-party audits covering security, availability, processing integrity, confidentiality, and privacy
- Enforce access controls, encryption, and data backups
- Implement incident response plans and log monitoring
- Conduct regular staff training on security protocols
- Maintain detailed audit trails and evidence for compliance
Our SOC 2 Type II Compliance Partners
ISO 27001
Demonstrates a globally recognized commitment to managing healthcare data risks.
Non-Certification Risks
- Contract losses due to lack of recognized security standards
- Increased breach risk from unstructured security practices
- Reputational damage from non-conformity during client/vendor reviews
- Regulatory scrutiny in case of security incidents
- Loss of competitive edge in global or enterprise healthcare markets
Why It’s Required?
- Proves a systematic approach to information security
- Strengthens risk management and threat mitigation
- Builds trust with healthcare clients and partners
- Ensures confidentiality, integrity, and availability of PHI
- Aligns with global data protection standards and HIPAA
Certification Process
- Develop and maintain an Information Security Management System (ISMS)
- Perform regular risk assessments and internal audits
- Define and enforce access control and data encryption policies
- Conduct continuous monitoring and incident response simulations
- Maintain third-party ISO 27001 certification via accredited bodies
Our ISO 27001 Certification Partners
FDA 510(k) Clearance
Proves your software is safe and effective for clinical use under FDA regulations.
Risks of FDA 510(k) Non-Clearance
- Prohibited from legally marketing or distributing the product
- Risk of FDA enforcement actions, including seizure or injunction
- Civil or criminal penalties in case of unapproved software use
- Loss of provider confidence in uncertified clinical features
- Significant delays in product launches or go-to-market timelines
Why It’s Required?
- Required for Software as a Medical Device (SaMD) classification
- Enables legal market entry for clinical decision support tools
- Demonstrates safety, efficacy, and substantial equivalence
- Builds trust with providers and patients using regulated features
- Reduces legal and regulatory exposure in case of adverse outcomes
Clearance Process
- Determine if the software qualifies as a regulated medical device
- Conduct risk classification and predicate device comparison
- Prepare technical documentation and usability validation
- Submit 510(k) premarket notification to the FDA
- Support post-market surveillance and updates after clearance
Our FDA 510 (k) Compliance Partners

Why Thinkitive is the #1 Choice for Custom EHR Software Development
10+ years exclusively in healthcare technology with 500+ successful custom EHR development projects.
![]() Tailored to Your Needs
Tailored to Your Needs
Thinkitive’s first step to developing ... customizable EHR software is to understand your unique needs and requirements. Based on that, our development team develops a customized software solution to meet your requirements and solve your problems.
![]() Ready-to-Use Components
Ready-to-Use Components
With our ready-to-use technology components ...like video conferencing, appointment scheduling, and SOAP notes, fasten your custom EHR Software development process.
![]() Third-Party Integration
Third-Party Integration
Integrate your EHR software system with ... multiple third-party systems like Telemedicine, RPM Devices, Labs, Radiology, etc., to build a complete virtual healthcare ecosystem.
![]() Affordable EHR Solutions
Affordable EHR Solutions
With our ready-to-use base EHR software framework, ...we present you an affordable primary care EHR software development which is specially curated for your healthcare practice.
![]() In-Depth Domain Expertise
In-Depth Domain Expertise
We have expertise in HIPAA-compliant ...primary care EHR development that provides flexible, scalable, and robust solutions.
![]() Timely Delivery
Timely Delivery
WWe have curated an EHR system development ...process that covers all the aspects of your healthcare practice’s unique needs and requirements with transparency for on-time delivery.













