Meet All Required Healthcare Compliance Standards Through Custom EHR Development
Build your EHR on a solid foundation of HIPAA, ONC, and all necessary security standards for a secure, reliable system
HIPAA Compliance
Protect patient health information by adhering to strict privacy and security safeguards
- Tier 1: Unaware of violation — $141 to $71,162 per violatio
- Tier 2: Reasonable cause (not willful) — $1,424 to $71,162 per violation
- Tier 3: Willful neglect, corrected — $14,232 to $71,162 per violation
- Tier 4: Willful neglect, not corrected — $71,162 to $2,134,831 per violation
- Annual Maximum: $1.5M (Per Violation Type)
- Expands and strengthens HIPAA enforcement
- Requires breach notification to patients and HHS
- Promotes secure EHR adoption and meaningful use
- Enables State Attorneys General to file HIPAA lawsuits
- Boosts patient confidence in digital health systems
- Conduct EHR system audits for compliance gaps
- Encrypt all stored and transmitted ePHI
- Establish breach detection and reporting procedures
- Train staff on HITECH-specific privacy/security updates
- Maintain detailed documentation for audit readiness
Our HIPAA Compliance Partners
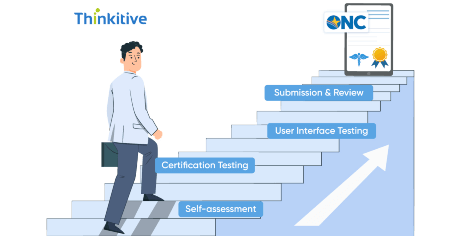
ONC Certification
Ensures that your EHR meets federal standards for safety, usability, and interoperability
- Using uncertified EHR systems - Ineligible for CMS. incentives (MIPS, Medicaid PI).
- Certification non-compliance - Subject to CMS payment adjustments or scoring penalties
- Vendor decertification - Removal from CHPL and reduced provider trust
- Repeat violations or program exclusion - Long-term loss of eligibility and reputational harm
- Required for participation in federal incentive programs (like Promoting Interoperability)
- Demonstrates compliance with national standards for security and interoperability
- Enhances trust among providers, payers, and patients
- Enables seamless data exchange between providers and health systems
- Protects your reputation by aligning with a federally approved certification
- Choose an EHR system certified under the ONC Health IT Certification Program
- Ensure compliance with 2015 Edition Cures Update criteria (including FHIR APIs)
- Verify support for clinical quality measures and interoperability standards
- Implement Real World Testing and attestations as required
- Partner with a vendor experienced in certified EMR development and maintenance
FHIR/HL7
The modern backbone of real-time, interoperable healthcare data exchange
- Poor compatibility with apps and systems
- Integration breakdowns and data silos
- Non-compliance with CMS/ONC rules
- Regulatory attention and data blocking risks
- No readiness for AI, remote care, or digital growth
- Required under CMS and ONC Interoperability mandates
- Enables seamless data exchange between systems, payers, and patient-facing apps
- Future-proofs your EHR system for upcoming regulations and digital health innovation
- Enhances patient access to data via standardized APIs
- Supports integration with 3rd-party tools, remote monitoring, and care coordination apps
- Adopt FHIR-based APIs as per the ONC 2015 Cures Update criteria
- Map clinical and administrative data to FHIR resource models
- Ensure secure authentication (e.g., SMART on FHIR, OAuth 2.0)
- Test interoperability with external systems, apps, and payers
- Monitor compliance with CMS and ONC guidelines around data exchange and access
Our FHIR-HL7 Compliance Partners
21st Century Cures Act
Empowers patients with data access and drives interoperability across systems
- Up to $1M per violation for EHR developers, HIEs, and HINs engaged in information blocking
- Loss of CMS incentives for non-compliant providers
- Zero score in the MIPS Promoting Interoperability category
- Reduced Medicare payments to hospitals and CAHs
- Exclusion from ACO participation for at least one year
- Mandated by ONC and CMS for patient access to records
- Drives transparency and patient-centered care
- Requires seamless API access to health information
- Enables compliance with FHIR and SMART on FHIR standards
- Essential for future CMS reimbursement and program eligibility
- Enable API-based access to EHR data as per the Cures Act Final Rule
- Prevent information blocking through clear data-sharing policies
- Adopt certified EHR technology that meets the ONC 2015 Cures Updatet
- Train staff on permissible exceptions and patient data rights
- Monitor compliance, patient access logs, and information requests
Our 21st Century Cures Act Compliance Partners
Medical Coding Standards
Standardizes clinical language to ensure accurate billing, reporting, and care
- Claim denials or delays due to incorrect CPT/ICD codes
- Revenue loss - reimbursement underpayments and recoupments
- Audit exposure from CMS or payers triggered by miscoding
- False Claims Act liability for upcoding, unbundling, or misrepresenting services
- Exclusion from Medicare/Medicaid for persistent violations of NCCI or coding rules
- Ensures accurate medical billing and prevents claim denials
- Supports timely reimbursements from insurers and CMS
- Reduces risk of fraud investigations and legal exposure
- Maintains payer trust and long-term contract eligibility
- Enables compliance with national coding updates (e.g., CMS, AMA).
- Implement automated coding validation tools
- Stay aligned with CMS and AMA coding updates
- Regular internal audits and coding reviews
- Train staff on evolving coding standards and edits (e.g., NCCI)
- Integrate intelligent prompts into EHR for real-time support
Our Medical Coding Standards Adherence Partners
SOC 2 Type II Certification
Validates your system’s operational security, availability, and data integrity controls
- Loss of business contracts due to security concerns
- Reputational damage from failed audits or data breaches
- Potential legal exposure in breach-related lawsuit
- Operational disruptions due to system downtime
- Reduced partner and payer confidence in your platform
- Demonstrates commitment to data security & integrity
- Builds trust with healthcare providers and partners
- Ensures safe handling of PHI and ePHI in cloud environments
- Strengthens resilience against breaches & system failures
- Aligns with HIPAA and industry-recognized security standards
- Conduct annual third-party audits covering security, availability, processing integrity, confidentiality, and privacy.
- Enforce access controls, encryption, and data backups.
- Implement incident response plans and log monitoring.
- Conduct regular staff training on security protocols.
- Maintain detailed audit trails and evidence for compliance.
Our SOC 2 Type II Compliance Partners
ISO 27001
Demonstrates a globally recognized commitment to managing healthcare data risks
- Contract losses due to a lack of recognized security standards
- Increased breach risk from unstructured security practices
- Reputational damage from non-conformity during client/vendor reviews
- Regulatory scrutiny in case of security incidents
- Loss of competitive edge in global or enterprise healthcare markets
- Provides a systematic approach to information security.
- Strengthens risk management and threat mitigation.
- Builds trust with healthcare clients and partners.
- Ensures confidentiality, integrity, and availability of PHI.
- Aligns with global data protection standards and HIPAA.
- Develop and maintain an Information Security Management System (ISMS).
- Perform regular risk assessments and internal audits.
- Define and enforce access control and data encryption policies.
- Conduct continuous monitoring and incident response simulations.
- Maintain third-party ISO 27001 certification via accredited bodies.
Our ISO 27001 Certification Partners
FDA 510(k) Clearance
Proves your software is safe and effective for clinical use under FDA regulations
- Prohibited from legally marketing or distributing the product.
- Risk of FDA enforcement actions, including seizure or injunction.
- Civil or criminal penalties in case of unapproved software use.
- Loss of provider confidence in uncertified clinical features.
- Significant delays in product launches or go-to-market timelines.
- Required for Software as a Medical Device (SaMD) classification.
- Enables legal market entry for clinical decision support tools.
- Demonstrates safety, efficacy, and substantial equivalence.
- Builds trust with providers and patients using regulated features.
- Reduces legal and regulatory exposure in case of adverse outcomes.
- Determine if the software qualifies as a regulated medical device.
- Conduct risk classification and predicate device comparison.
- Prepare technical documentation and usability validation.
- Submit a 510(k) premarket notification to the FDA.
- Support post-market surveillance and updates after clearance.
Our FDA 510 (k) Compliance Partners